Endourology
OVERVIEW
The field of Endourology deals with accessing and treating urinary tract disorders using the endoscopic equipment.
Benign Prostatic Hypertrophy (BPH)
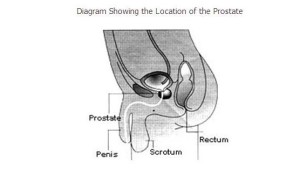
The prostate is a small, chestnut-shaped gland in the male
reproductive system. Only men have a prostate. It is composed of
different lobes enclosed in a fibrous capsule. Located in front of
the rectum and just below the urinary bladder, the prostate also
surrounds part of the urethra (the canal through which urine is
carried from the bladder and out of the body through the penis) as
shown in the diagram below. Diagram Showing the Location of the
Prostate

The prostate contributes to the milky fluid that carries the sperm produced by the testes. The prostatic fluid is also thought to supply nourishment for the sperm. Since the prostate contributes to ejaculation throughout the better part of a man’s life, many men are able to father children well into their 70s and 80s.
BPH is a non-cancerous enlargement of the prostate gland in men. BPH is commonly found in older men. Throughout childhood, the prostate is very small. It begins to enlarge during puberty and approximately doubles in size; then the growth slows down. At around the age of 45, the prostate often starts growing again and continues to enlarge for the rest of a man’s life. This is considered to be due to hormonal changes.
The enlargement itself is not the problem. However, as it continues to enlarge, it can frequently start to squeeze the urethra (this is similar to what happens when a straw is pinched). This can interfere with the normal flow of urine and cause uncomfortable symptoms. An enlarged prostate generally does not interfere with sexual functioning. However, severe urinary symptoms can be embarrassing and can inhibit a man’s sexual activity.
Not all males suffer from the symptoms of an enlarged prostate. 4 out of every 10 men over the age of 55, 7 out of 10 men in their 70s and an even larger number by the age of 80, suffer from the symptoms of an enlarged prostate.
The urinary symptoms of an enlarged prostate are one or more of the following:
- Frequent urination, especially at night
- A sudden, uncontrollable urge to urinate
- A poor urine stream
- A sense of the bladder not emptying completely
- Difficulty in starting urination
- Urinary incontinence
- Total blockage of urine
- Bleeding in the urine
- Urinary infection
BPH is usually diagnosed in the following manner or by a combination of some of the methods listed below:
Medical History: Your doctor will take a detailed medical history, which will include past and present medical problems.
Digital Rectal Examination: Examination of the prostate gland by inserting a gloved, lubricated finger into the rectum
Checking for Other Medical Problems: that may be causing similar symptoms.
Checking of Your Urine: for the presence of infection.
Performing a Urine Flow Test: for the measurement of urine flow. A flowmeter is used to measure the force of your urine stream and the degree of blockage.
- Performing an Ultrasound Scan: to obtain details about the prostate gland, its effects on the kidneys, if any, and the amount of urine in the bladder after urinating.
- Performing a Urodynamic Study: if needed, to check bladder pressure.
- Measurement of the Post-Voiding Residual Urine: (urine remaining in the bladder after urination or voiding) by catheterization or ultrasound.
- Ultrasound of the Urinary Tract
- Cystoscopy (Examination of the Urinary Tract with a Special Viewing Tube)
Depending on the severity of your symptoms, several treatment options are available. Your Urologist will discuss these options with you before deciding on any one method:
- Medical Management: These are suitable only for mild symptoms and when the degree of obstruction is not severe. These medications have to be taken life-long and have a proven benefit of only 20-30%. Depending upon the drug used, you may experience minor side effects. Drugs such as 5 alpha-reductase are supposed to act by reducing the size of the enlarged prostate over a long-term period. These, however, are not suitable for all types of prostates. Other drugs, such as alpha-blockers, relax the smooth muscle component in the region of the prostate and partially open up the passage. These provide only symptomatic relief.
Surgical Management: is currently the best method of treatment. A surgical procedure called TURP is performed:
- TURP (Transurethral Resection): of the prostate is the gold standard among various surgical options. TURP is a procedure used to resect the prostate that may be enlarged due to benign prostatic hypertrophy (BPH). During TURP, an endoscope is inserted through the penis into the urethra (the urinary passage), and the innermost core of the gland adenoma is removed. This widens the passage and relieves the compression on the urethra. This may be likened to removing the meat of an orange while leaving the skin intact. The operation takes about half an hour to two hours, with no incision on the skin.
For large prostates more than 100 gm, HOLEP is recommended.
The possible post-operative effects of this surgery, in some cases, may include:
- About 50% of patients experience failure to ejaculate after intercourse, as the semen is pushed backward into the bladder, instead of to the outside.
- Very rarely, some people experience leakage of urine either upon straining or continuously
- About 2% of patients may experience transcend or permanent impotence.
All tissue removed at the time of surgery will be sent for examination to confirm the benign nature of the gland. Very occasionally, a surprise report of the presence of malignancy may be obtained.
Treatment for BPH does not eliminate the future incidence of Prostate Cancer as this originates in an entirely different portion of the gland. Therefore, an annual evaluation may still be considered important for men who have undergone surgery for benign prostate gland enlargement.
Just because the prostate is enlarged, it does not need to be treated. If your symptoms are mild, you may not need any treatment at all. If your symptoms are severe or if the result of the tests shows that the urinary tract is significantly affected, you must undergo early therapy.
PCNL is a procedure for removing stones in the kidney or the upper ureter
Illustration Showing How PCNL is Performed

PCNL is a well-established procedure by which stones in the kidney or the upper ureter are removed by making a small incision in the flank. Generally, an incision, that is 1 cm or less than 1 cm, is made in the flank. A guide wire is passed through this incision into the kidney. This is performed under fluoroscopy or x-ray control.
A passage is then created around this guide wire by dilatation. Through this passage, a nephroscope is passed into the kidney to visualize the stone and remove it. Larger stones can be fragmented by different methods and removed. Stones are therefore cleared easily. Once the procedure is complete, a tube is left through this track as drainage for one or two days.
The main advantage of this approach is that, unlike traditional open surgery, only a 1 cm incision is made in the flank. The stones can be visualized directly and removed. Unlike ESWL or ureteroscopy, the stones are removed in the same sitting and the kidney is cleared of calculi. The stay in the hospital is only for 3-4 days.
This surgery would be recommended as a treatment of choice if the patient has kidney stones larger than 2 cm, upper ureteric stones bigger than 1 cm or at times for stones found in the lower pole of the kidney that cannot be effectively treated with either ureteroscopy or ESWL. This procedure is also performed following the failure of other modalities of treatment such as medical therapy, ESWL, etc., for renal and upper ureteric stones.
This procedure is commonly performed under general anaesthesia, and therefore you also need to be admitted to the hospital for this procedure. In special circumstances, it can be performed under intravenous sedation, regional anaesthesia or local anaesthesia.
The success rate of clearance of stones with this procedure ranges between 90 to 95%. This actually depends upon the size, number and location of these stones. Sometimes, complete clearance may require a second procedure after a few days.
For the post-operative course, the patient will generally need to stay in the hospital for 2 to 3 days after the procedure. He or she will also undergo additional x-rays or ultrasound studies, to determine if there are any residual stone fragments present. A large amount of residue will require the urologist to look again with a nephroscope to remove it. The other alternative is to treat the remaining fragments with ESWL. From the site of the puncture, the patient will have a drainage tube and a urethral catheter, for a day or two. Following the removal of the flank drainage tube, urine may leak for a day. Post-operatively, the Urologist will also encourage a high fluid intake to keep the daily volume of urine produced to more than 2 liters a day.
By and large, this procedure is safe. Some risks that can be associated with all surgical procedures are the possibilities of bleeding (1%) and infection, sometimes requiring a blood transfusion.
Some patients have prolonged leakage of urine from the flank site, requiring ureteric stenting. Fever, if present, will require a change in antibiotic.
The entire gamut of paediatric endoscopes for both the upper and lower tracts is available. These include cystoscopy, resectoscope, urethrotome, ureteroscope and nephroscope. We are one of the few centers that are equipped to operate on the entire range of Paediatric Urology disorders.