What is urotherapy counselling?
Urotherapy is a non-invasive recommendation traditionally used in the management of dysfunctional voiding and irregular bowel movement habits.
What is Dysfunctional voiding?
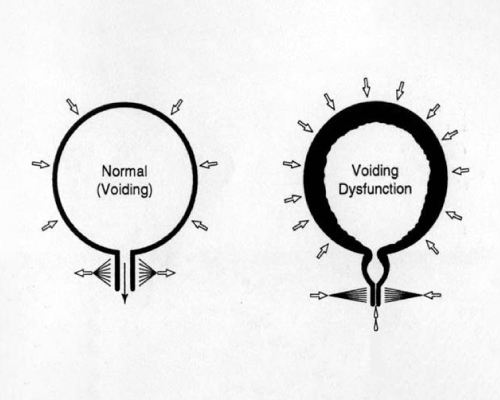
With normal urination, the urethral sphincter relaxes and opens out when the bladder muscle squeezes, allowing urine to pass out of the body freely.In those with dysfunctional voiding, the urethral sphincter does not relax when the bladder muscle squeezes, making it difficult for urine to be expelled out against an obstruction. This will increase the bladder pressure and change the micro organic climate of the urinary bladder thereby resulting in urinary tract infection.
What happens in an irregular bowel movement habit?
An irregular bowel movement will result in impacted stool in the rectum which compresses the bladder, reduces its functional capacity, and provokes earlier sensation to void. In addition, to retain stools in the rectum, there will be chronic pelvic floor spasm which also prevents complete relaxation during voiding, and can result in post void residuals. As the pelvic floor muscles are common to both the urine outflow and bowel control, this can aggravate dysfunctional voiding.
Why is urotherapy done?
The primary aim of the therapy is to normalize the bladder and bowel function. This therapy also aims at improvement of quality of life.
What does urotherapy involve?
Urotherapy involves the following;
Maintaining urine storage volumes to within the safe capacity of each individual’s bladder.Emptying the bowel regularly so that the impacted stool does not exert pressure over the urinary bladder and also facilitate pelvic muscle relaxation. Maintaining void volumes/timings to safe limit, so as to let the pelvic/urethral muscles relax periodically. Use of medications like anticholinergics and laxatives, if required.
Who performs this therapy?
Your doctor or a trained nurse counsellor will explain to you all the recommendations after assessing your clinical condition.
What are the recommendations?
In fact, recommendations will depend on the assessment results of your doctor/nurse counsellor. They may be as follows:
- Tailoring of fluid consumption according to age, occupation, daily activities, and climatic condition to prevent the bladder become over distended frequently. This includes all kind of drinks also, like coffee/tea, milk, juice etc. Your doctor/nurse counselor will tell you how much of fluid is to be taken for a day. This should be distributed over 24 hours.
-
- Timed urination in the daytime. Practising timed emptying of the bladder every three hours will keep the urine stored in the bladder at low pressures. You may have to do that with an alarm, if you are likely to be engaged with work
- Pass urine before going to sleep and immediately on getting up
- Pass urine once in the night. Use an alarm to wake you up three hours after you go to bed
- Maintain an interval of 2 hours between dinner and sleep, to facilitate removal of dietary liquids
- Increase the fiber content of food in the daily diet. It includes:
- All unrefined/unsieved cereals (Roti, Chapathi)
- All Dhals, Beans, Lentils (whole- grams, sprouted grams), fresh peas
- Green leafy vegetables, Raw vegetables (should be just cooked, not over cooked)
- All fruits with edible portion of peel/skin
- Restriction of fluid consumption in the evenings to decrease the overnight urine output would be another advice
- Ensure you pass stools daily, at fixed times, preferably before you get occupied with the days activities.
What next?
You will be asked to come back after a certain period, usually one month, with 3 days of bladder diary to judge your compliance to our advice. A bladder diary records the time you get up and the time you go to bed, fluid intake, frequency of urination, urinated volumes and other information such as degree of urgency, episodes of leak etc. You will be trained by your nurse counselor on how to maintain a bladder diary.