Kidneys are small bean-shaped organs, each about the size of a fist. They are located on either side of the spine at the lowest level of the rib cage in the abdomen. Each kidney consists of about a million filtering units called "Nephrons".
Medical Tourism
Kidneys are small bean-shaped organs, each about the size of a fist. They are located on either side of the spine at the lowest level of the rib cage in the abdomen. Each kidney consists of about a million filtering units called "Nephrons". The main function of the kidney is to filter waste products from the blood. Approximately, 150 liters of fluid is filtered by the kidney each day. 148.5 liters of the filtered fluid is recovered and the remaining 1.5 liters is excreted as urine. The urine is sent to the urinary bladder where it can be stored anywhere between one to eight hours. The production of urine involves complex steps of filtration, secretion, and reabsorption.
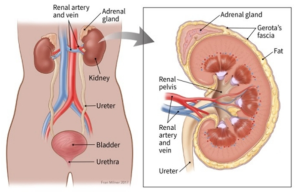
Fig. 1 – Urinary system and cut section of kidney
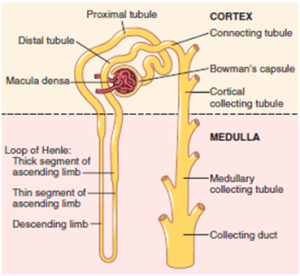
Fig 2 – The Nephron
Functions of The Kidney
1. Removes waste products from the body 2. Removes drugs from the body 3. Balances the body fluid 4. Releases hormone that regular blood pressure 5. Produces active vitamin D needed for bone health 6. Control production of red blood cells
Kidney Disease
There are two main types of kidney disease. Acute Kidney Injury (AKI) and Chronic Kidney Disease (CKD). Acute kidney injury occurs suddenly and recovers completely on most occasions. It is caused by insults to the kidney from infections, drugs, toxins, obstruction to urine flow to name a few. Once the inciting cause is treated appropriately, the kidneys recover. However, AKI can also lead to chronic kidney disease in a few instances. Temporary dialysis support may be required in some patients with AKI. Chronic kidney disease is defined as having structural damage or decreased function for three months or longer. The hallmark of CKD is inexorable progression overtime and irreversibility. Prevention should be the main focus as there is no cure for CKD.
Causes Of Chronic Kidney Disease
The major causes of CKD are Diabetes and Hypertension. The other causes include glomerulonephritis, inherited kidney disease (Polycystic Kidney Disease, Alport's syndrome, Primary Hyperoxaluria), recurrent urinary tract infections, long-standing obstruction to urine flow (stones, prostate gland enlargement) and drugs and toxins. CKD can also occur because of a variety of immunological disorders like Systemic Lupus Nephritis (SLE), vasculitis, etc.
Symptoms of CKD
Chronic Kidney Disease is usually silent, and symptoms are very nonspecific. Periodic testing is necessary especially in individuals at risk to detect it early. A number of symptoms can develop in the later stages of kidney disease. Symptoms can include - Weight loss and poor appetite - Swelling of feet or hands - Shortness of breath - Tiredness - Blood in urine - Frequent urination at night - Difficulty in sleeping - Itching - Muscle cramps - Nausea or vomiting - Sexual dysfunction
DIAGNOSIS OF KIDNEY DISEASE
Kidney disease can be diagnosed with blood and urine tests. In many cases, it is picked up because routine blood or urine test indicates kidney disease. Regular testing is recommended if one has: - Hypertension - Diabetes - Heart disease - A close family member has chronic kidney disease - Age over 55 years - Other conditions affecting kidneys like kidney stones, enlarged prostate or SLE - Acute kidney injury - Protein or blood in urine without any known cause - People taking long-term medications that can affect kidneys such as lithium, NSAIDs, etc. The main test for kidney disease is measuring the level of creatinine in the blood. Using this result, a calculation that takes into account age, gender, and ethnicity is dyspnea on exertion to estimate the filtering capacity of the kidney. This is known as estimated glomerular filtration rate eGFR. The kidney disease is staged based on eGFR.
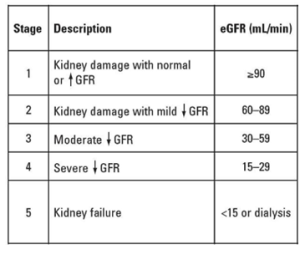
Table 1 – Stages of Chronic Kidney Disease Urine is checked for the presence of protein in the blood. The other tests include: Ultrasound scan of the kidneys to check how the kidneys look like and check whether there are blockages. Kidney biopsy – a small sample of kidney tissue is removed using a needle and is examined under a microscope.
Diabetes and Kidney Disease
Diabetes is the single most common cause of chronic kidney disease. about 30% of patients with Type 1 diabetes (juvenile onset) and 10 to 40% of patients with type 2 diabetes (adult onset) develop CKD. Diabetes causes injury to the small blood vessels of the body. When the blood vessels in the kidneys are injured, the filtration function is affected and protein leaks into the urine. Over time, waste products including salt and fluid accumulate in the body resulting in leg swelling and kidney failure. The other ways in which diabetes can cause kidney disease is by damage to the nerves causing difficulty in emptying the urine from the bladder. The resulting pressure from a full bladder can back up and injure the kidneys. Recurrent urinary infections can also be the cause of kidney damage. It is proven that tight diabetes control reduces the risk of developing kidney disease significantly (Fasting blood sugar < 100mg/dl; Post Prandial blood sugar <140mg/dl; HbA1c < 6.5%).
Hypertension and Kidney Disease
Hypertension is defined as blood pressure of over 140/90 mmHg. Hypertension may be the cause or consequence of chronic kidney disease. High blood pressure causes stretching of blood vessels. It is called shear stress in Physics. The stretching eventually scars and weakens blood vessels throughout the body including those in kidneys. This impairs the ability of kidneys to remove waste and fluid from the body. Extra fluid in the body may then raise the blood pressure, even more, creating a vicious cycle. This leads on to kidney disease and ultimately kidney failure. Hypertension is the second major cause of CKD.
Obesity And Kidney
Obesity is a medical condition marked by the accumulation of excessive body fat with negative health impacts. It is generally reported in terms of Body Mass Index (BMI) a value obtained by dividing weight by the square of the height (BMI = Weight (Kg)/{Height) 2cm). BMI of over 30 kg/m2 is considered obese and 25-30 kg/m2 is overweight. The cause is a combination of excessive calorie intake, sedentary lifestyle, and genetic susceptibility. It is a risk factor for developing various diseases like type 2 diabetes, osteoarthritis, certain cancers, and depression. Today we have more overweight and obese people than ever before. In the USA, 70% of Americans over 20 years of age are overweight and about a third of them are obese – unfortunately, the problem is much more common in children too. India is a developing nation. It is struggling with poverty, malnutrition, and disease. Surprisingly, we have the second highest number of obese children in the world (14.4 million). Indian obesity is marked by the thin-fat Indian Phenotype. Abdominal obesity and visceral fat are striking. The BMI threshold should be 25 kg/m 2 for Indians. Obesity is associated with a kidney condition called focal and segmental glomerulosclerosis (FSGS). Of late, the incidence of this disease has increased in tandem with obesity. The cause is likely to be due to the insulin resistance/hyperinsulinemia causing injury to the blood vessels of the kidney.
Drugs and Kidney Disease
Kidneys provide the final common pathway for excretion of many drugs. Therefore, they are exposed to high concentrations of potentially toxic substances. This causes damage to the renal tubular cells and papillae. Minor damage may pass undetected. Toxicity tends to be dose-dependent. The ill effects of drugs are more in patients with pre-existing kidney disease. Drugs can cause both AKI and CKD. The ill effects of drugs on the kidney can be categorized as follows: Prerenal effects Obstruction to flow of urine Allergic or immunological damage Direct cell toxicity
The following groups of drugs are commonly associated with kidney damage:
- Antibiotics are given for infections (gentamycin, amikacin, quinolones) - Diuretics or water pills - Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) or painkillers - Proton Pump Inhibitors giver for gastritis, ulcers etc - Slimming Pills - Radiocontrast Dyes used in CT Scan and Angiograms
Tubulointerstitial Disease of The Kidney
Tubulointerstitial nephritis (TIN) is a frequent cause of acute kidney injury (AKI) that results in CKD. TIN is a result of immunological injury to the kidney tubules and interstitium which may progress to fibrosis (scarring). The causes include infection, drugs, genetic conditions, idiopathic (unknown cause) or related to a systemic inflammatory condition. The disease can be silent without any symptoms when caused by an allergic reaction the usual symptoms are fever (27% patients), rash (15% of patients) and enlarged kidneys. About a quarter of them have high levels of eosinophils in the blood. Urine examination finding includes eosinophils, blood, pus cells, and proteins. The mainstay of treatment is removing the offending agent. Corticosteroid has been used but there is no clear evidence that it helps. The kidney function can be only slightly affected, but at times it may fail completely needing dialysis. The kidney biopsy is done in patients to diagnose it. In most cases of acute TIN, the kidney function will return back. Chronic TIN has no cure. It progresses over time and eventually, patients may require dialysis and transplantation.
Polycystic Kidney Disease
This disease is characterized by the presence of numerous cysts in the kidneys. These cysts are filled with fluid. If there are too many cysts or if the cysts get too big, the kidneys get damaged. The cysts can replace much of the kidney or can damage by exerting pressure on the tissue resulting in kidney failure. It is a genetic kidney disease. The genes determine the likelihood of developing this disease. It causes about 5% of all kidney failure. Besides the kidney, patients with PKD can develop cysts in the other abdominal organs too. But these cysts do not cause serious problems. Some patients develop a bulging vessel inside the brain called aneurysm. This vessel can burst to result in a stroke or even death. Floppy heart valves, hernias are also common in PKD. The symptoms usually develop by the third or fourth decade. Usual symptoms are back pain, high blood pressure, blood in urine, and frequent urinary infections. Ultrasonogram is the most reliable, inexpensive, and non-invasive mode of diagnosis. CT scan/MRI are at times done to measure the volume and growth of kidneys and cysts. Genetic testing for the abnormal gene is now widely available. It is not recommended for everyone or it is costly and fails to diagnose the disease in 15% of people. However, genetic testing will be useful when - Diagnosis is not clear on imaging tests - One has the family history of PKD and wants to donate the kidney. As with other cause of CKD, there is no specific treatment for PKD too.
Kidney Disease Is A Lifestyle Disease
Most of the disease-causing CKD can be to a great extent attributed to the lifestyle of the population. Sedentary lifestyle, unhealthy eating habits, obesity, excessive use of over-the-counter drugs, smoking, alcohol intake, and stress are some of the main reasons. It is high time that we all change our lifestyle to reduce the burden of such non-communicable diseases. After all, "Health is Wealth."
Treatment of CKD
There is no cure for CKD, but treatment can help relieve symptoms and slow progression of CKD. Treatment depends on the stage of CKD. The main treatments are, - Lifestyle changes - Medications – to control associated problems like diabetes, hypertension, high cholesterol, anemia, etc. - Dialysis - it is done in advanced stages (CKD 5) of CKD - Kidney transplantation – it is done in advanced stages of CKD (CKD 5)
Life Style Changes
- Quit smoking if one is a smoker - Restrict salt intake to 4g per day - Regular exercise - Lose weight if one is obese or overweight - Avoid over-the-counter NSAIDs like ibuprofen - Consult doctor and dietician regarding the diet suitable for the stage of CKD
MEDICATIONS
There are no medicines specifically for CKD. Medicines are usually prescribed for complaints of existing conditions like hypertension, diabetes mellitus, high cholesterol, phosphate binders, erythropoietin, etc.
Dialysis:
This is required when the kidney function is no longer able to sustain the bodily functions. This rarely happens all of a sudden, so there is enough time to plan the treatment. It is advisable to get an AV fistula created as and when advised by the nephrologist. There are two types of dialysis Hemodialysis: The blood is diverted into an external machine, where it is filtered before being returned back to the body. It requires access to the blood circulation. The main types of access are temporarily (tunneled and non-tunneled catheter into a central vein) and permanent (AV fistula/AV graft). It is best to start dialysis with a functioning permanent vascular access. The procedure is done thrice weekly. Each session lasts for about 4-5 hours. A blood thinner is used to prevent clotting of blood in the external circuit during the procedure. Hemodialysis is done in the hospital or at home.
Peritoneal Dialysis:
2-3 liters of fluid is let into the abdomen through a catheter. The dialysis occurs from the blood vessels lining the inside of the abdomen called peritoneum. It can be performed manually or using a machine. If done manually (CAPD – Chronic Ambulatory Peritoneal Dialysis) 3-4 exchanges are to be done each lasting for 4-8 hours each. It is performed by a machine (APD automated Peritoneal Dialysis). It is done overnight for about 10 hours using 10 liters of fluid. Peritoneal dialysis is done at home. Dialysis needs to be done lifelong or until one gets kidney transplantation.
Kidney Transplant:
This is the natural treatment of CKD wherein a normally functioning kidney from a healthy living donor or a brain-dead person is surgically placed in the lower abdomen. It is often the most effective treatment too. A human body has the capacity to identify self from non-self. It tries to attack and damage anything that is foreign. Hence medications are given to suppress the immune system to prevent rejection of the transplanted kidney. These medications need to be taken for the rest of one's life. Survival rates for kidney transplants are extremely good. The success rates are 93-95% for the first years, 85% for five years, and many functions after 10 years or more. Living donor kidney transplantation is the most common form of transplant in India. Deceased donor transplant program is slowly on the rise. Few states like Tamil Nadu, Gujarat are performing a lot of deceased donor renal transplants compared to the other states. The law permits organ donation from blood relatives (parents, siblings, children, grandparents) and from spouses. Blood group compatibility was a must a few years ago for renal transplantation. Today, blood group incompatible transplantation is feasible and being done in many centers across India. Except for the increased risk of rejection in the initial 1 month the long-term outcome is comparable to ABO-compatible transplants. To perform a renal transplantation approval is required from the respective state governments. To make the process easier, high volume centers have been given the authority to approve living related donor transplantation. The onus is on the family to give the proof of relationship in addition to the tissue matching and DNA fingerprinting tests which are done as a routine. The required documents are to be submitted along with all the lab reports to the appropriate authority. The committee then interviews s the potential donor and the recipient. If they are convinced of the altruism, a letter or approval is issued to the transplant center to proceed with the transplantation. Foreign nationals can get living donor renal transplantation in India. A more elaborate procedure is to be done including approval from the respective nation’s high commission. Once all the testing is done and the donor is found suitable, the documents are sent for approval from the state authorization committee. It is only after approval that the transplantation should be carried. The transplant coordinator of the hospital will be able to guide the patient in the process.
Prevention of Kidney Disease:
Kidney disease is often silent until very advanced. There is no cure for CKD. Prevention is the key. Early detection of kidney disease and referral to a Nephrologist will help a patient in retarding the disease progression and planning of the treatment of CKD stage 5. People at risk for CKD need to get annual screening or more frequently as deemed by their Physician. A simple blood and urine test along with BP measurement is enough. The following are some tips to prevent kidney disease: • Good control of Diabetes and high blood pressure • Take the prescribed medicines without fail • Do not miss appointments with the doctor • Quit smoking • Lose weight if overweight or obese • Cut down on salt intake • Regular physical exercise • Ensure adequate fluid intake • Avoid over the counter medications especially painkillers.
Urologists and Nephrologists:
Urologists and Nephrologists both treat kidney problems. Urologists are surgeons who focus on structural disorders of the kidneys and urinary tract. They treat problems like kidney stones, kidney cancer, obstruction to urine passage, prostate diseases to name a few. They perform surgeries including kidney transplantation. Nephrologists are physicians who focus on disorders that affect the kidney function like glomerulonephritis, diabetes, hypertension, Polycystic kidney disease, AKI, and CKD. They handle dialysis and manage kidney transplant patients.