Paediatric Urology
OVERVIEW
Paediatric Urologists are the surgeons specialized in treating, diagnosing and managing urinary and genital related problems of children.If a child has a disease or, illness related with urinary tract (bladder, kidneys, ureters) or, genitals then it can be cured by a qualified and experienced paediatric urologists.
Types of treatment for children provided by a Paediatric Urologist
- Surgical management and evaluation of kidney stone disease
- Surgery for varicocele, hydrocele or, hernia, undescended testis
- Evaluation as well as management of vesicoureteral reflux, voiding disorders, and urinary tract infections
- Surgical reconstruction for urinary tract that involves bladder, ureters and kidneys that includes PUJ Obstruction, Ureteric Reimplant, Hypospadias, genital abnormalities and disorders related with sexual development.
- Evaluation as well management for urinary tract related problems that may be associated with neurological conditions(e.g; Spina bifida)
- Surgical management of the malignancies of the bladder, testis and kidney
How to find and where to consult a Paediatric Urologist-
Paediatric Urologists of NU Hospitals are the most sought after in Bengaluru.(Tab to submit form or, contact details or, Consult with hyperlink redirecting to form submission)Why to consult a Paediatric Urologist at NU Hospitals:
Children cannot tell what exactly is bothering them. They cannot answer medical related questions. They may not even be cooperative during the medical examination.Paediatric Urologists are the specialists who are trained to provide focused care on the special needs of children. They interact with the parents well. They know the methods that make children relaxed and cooperative during the examination. Qualified Paediatric Urologists use the equipment that is designed for children.
Paediatric Urology services offered at NU Hospitals:
- Paediatric Kidney Transplants
- Congenital Uro-Genital Anomalies correction
- Bedwetting(Nocturnal Enuresis)
- Hypospadias Repair
- Undescended Testis
- Congenital Obstruction of Urinary Tract
- Recurrent Urinary Tract Infections
- Paediatric Urodynamics and Neurourology
- Paediatric Kidney Stones Management
- Reconstructive surgeries of the Genito-Urinary Tract
- Paediatric Laparoscopic Urological Surgeries
- Paediatric Robotic Urological Surgeries
- Pyelopasty and Ureteric Reimplant
- Paediatric PCNL for Stone Disease
- Bladder Reconstruction
Who is a Pediatric Urologist?
If your child has an illness or disease of the genitals or urinary tract (kidneys, ureters, bladder), a Paediatric Urologist has the experience and qualifications to treat your child.
Children are not small adults. They cannot always say what is bothering them. They cannot always answer medical questions and are not always able to be patient and cooperative during a medical examination.
Pediatric Urologists are trained to focus care on the special needs of children and their parents – even on potentially sensitive and embarrassing subjects related to genitalia and voiding problems. They know how to examine and treat children in a way that makes them relaxed and cooperative. In addition, Pediatric Urologists often use equipment specially designed for children. This helps create a comfortable and non-threatening environment for your child.
If your Pediatrician suggests that your child see a Pediatric Urologist, you can be assured that he or she has the widest range of treatment options, the most extensive and comprehensive training, and the greatest expertise in dealing with children and in treating children’s urinary tract disorders.
Pediatric Urologists are medical doctors who have had:
- At least 6 years of medical school
- One to 3 years of surgical residency
- At least 3 additional years of residency training in general Urology Health
- One to 2 years of additional fellowship training in Pediatric Urology
A Pediatric Urologist must devote a minimum of 75% of his or her practice to the urologic problems of infants, children and adolescents
Pediatric Urologists are surgeons who can diagnose, treat and manage children’s urinary and genital problems. Paediatric Urologists generally provide the following services:
- Evaluation and management of voiding disorders, vesicoureteral reflux and urinary tract infections that require surgery
- Surgical reconstruction of the urinary tract (kidneys, ureters and bladder) including genital abnormalities, hypospadias and disorders of sex development
- Surgery for groin conditions in childhood and adolescence (undescended testes, hydrocele/hernia, varicocele).
- Evaluation and surgical management of kidney stone disease
- Surgical management of tumours and malignancies of the kidney, bladder and testis
- Evaluation and management of urological tract problems identified before birth
- Evaluation and management of urinary tract problems associated with neurological conditions such as spina bifida.
Antenatal Hydronephrosis, which simply means fluid-filled enlargement of the kidney before birth, is detected in the foetus by ultrasound studies performed as early as the first trimester of pregnancy. In most instances this diagnosis will not change obstetric care but will require surveillance and possible surgery during infancy and childhood.
Possible Causes of Antenatal Hydronephrosis:
Blockage – This may occur at the kidney in the Uretero Pelvic Junction (UPJ), at the bladder in the Uretero Vesical Junction (UVJ), or, in the urethra (posterior urethral valve).
Reflux– Vesicoureteral reflux occurs when the valve between the bladder and the ureter is incompetent permitting urine to flow back into the kidney when the bladder fills or empties. Almost 75% of children outgrow this during childhood but need daily antibiotic prophylaxis to try to prevent kidney damage before they outgrow the reflux.
Duplications etc. Perhaps 1% of all humans have two collecting tubes from a kidney. These may show up on the foetal ultrasound. Occasionally patients with duplication have ureterocele, which is a balloon-like obstruction at the end of one of the duplex tubes.
A multicystic kidney is a non-functional cystic kidney.
Normal Variant: Many of the dilated kidneys are found to be normal after delivery. It is likely that the dilation was due to the high urine output in the foetus and also because of the changes that occur in the kidney during development. Minor dilation of the kidney before birth does not always need evaluation after the child is born.
Management during Pregnancy: In nearly all instances of Antenatal hydronephrosis, ultrasound surveillance is all that is necessary. In the rare foetus with severe obstruction of both kidneys and insufficient amniotic fluid, drainage of the kidneys or bladder by tube or operation has been performed experimentally. For most cases of Antenatal Hydronephrosis pregnancy is not affected and delivery can be performed normally.
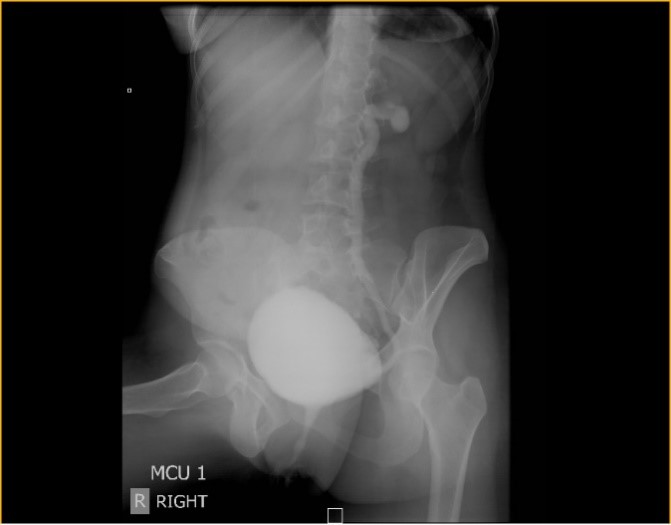
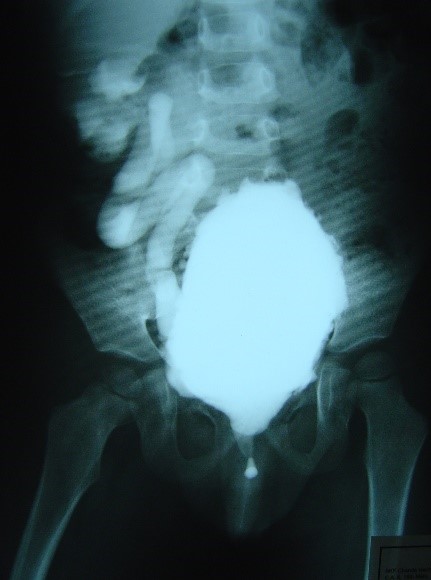
Management after birth: Postnatal ultrasound is usually performed before the child leaves the hospital. Voiding Cystourethrogram (VCUG), which requires a catheter in the bladder, is performed to exclude vesicoureteral reflux. This occurs in 25-30% of children with antenatal hydronephrosis. Obstruction is excluded with a diuretic renal scan (requiring an IV and a catheter). The renal scan is more accurate if delayed until the baby is one month of age,
Children with vesicoureteral reflux are managed with antibiotics and surveillance with periodic ultrasound and voiding cystogram. Children with an obstruction or blockage of the urinary tract may require surgical correction. In some babies, the evidence for obstruction is marginal or the degree of blockage is mild. In these babies, the tests might be repeated after a few months.
A multicystic dysplastic kidney doesn’t function, but the opposite kidney is usually normal. There exists an argument about whether a multicystic kidney should be removed or left alone. Unless it is causing a problem with mass effect, pain or discomfort, and if is serially found to be enlarging during follow up raising suspicion of tumour or blockage, then nephrectomy (removal of the affected side kidney) is performed. Otherwise, it is usually left alone in infancy and followed-up with ultrasound at 6 months and a year after. Follow up to care opposite normal kidney is essential.
Circumcision is one of the oldest operations ever to be performed. Sometimes it is done because of a specific problem with the foreskin (prepuce) and other times it is performed routinely. Routine circumcision was once advocated for all newborn Males. This is now performed in about 65% of new-borns. Most boys will do fine later in life if their foreskins are not removed. Some may eventually need circumcision because of narrowing at the tip (phimosis), infections (posthitis or balanitis), or irritation. The foreskin may be a source for urinary tract infections, and circumcision may be a good idea in boys with any underlying kidney abnormality as it will help in proper analysis of the urine analysis.
In very young babies, circumcision is performed in the hospital or clinic with local anaesthesia and a clamp. Although it is a commonly performed procedure. It is technically difficult. It is not uncommon for there to be some redundant penile skin after newborn circumcision. As the child grows, this will become less noticeable. Adhesions of the foreskin to the glans, or head of the penis, are also very common. If there is significant scarring, these can develop into skin bridges. Simple adhesions will usually resolve over time, but the skin bridges will require surgical correction.
Other complications of circumcision include bleeding, infection, skin separation, narrowing of the urinary opening (meatal stenosis), concealed penis and urethral fistula. Every circumcision may not look exactly like the “ideal circumcision” in the mind of the family members. The main purpose of circumcision is to remove the preputial ring to permit exposure of the glans penis. This is more of a functional purpose than a cosmetic purpose and although we try to get a cosmetic result in line with familial expectations this is not always the case.
When a circumcision needs to be revised, we generally wait until the child is 6 months of age to minimize aesthetic risks. This is also the age that we will perform a first-time circumcision if it was not able to be completed in the newborn. The procedure is done under general anaesthesia in the outpatient surgery centre or hospital. Any adhesions or other abnormalities are corrected and the excess redundant foreskin is removed. The skin is closed with small absorbable sutures.
Antibiotic ointment or Vaseline is suggested to be applied to the glans with every diaper change after circumcision. This is required for at least a few months to try to protect the newly exposed meatus from diaper irritation.
Hypospadias is a birth defect found in boys in which the urethral opening is not at the tip of the penis, but can be anywhere on the undersurface of the penis to the scrotum. Although a genetic factor exists in the development of hypospadias, no single cause has been identified. Bending of the penis on erection may be associated with this and is known as chordee. The overall incidence of hypospadias is about 8.2 in every 1,000 male births. There is some family risk of hypospadias. When we see a boy with hypospadias there is a 15% chance of finding this in another family member such as a father or brother. There are different degrees of hypospadias, some minor and others more severe. In most children, the opening of the urethra is near the end of the penis. We name the types of hypospadias according to their anatomic location, which may be near the tip of glans penis or near the anal opening (perineal). And it is necessary to determine whether or not there is associated chordee and this will determine the type of surgery needed and if the surgery can be completed in one stage or two stages.
Some children may have chordee without hypospadias. The urethral opening in these patients is in the normal location.
Reasons for Correction
Surgical correction of hypospadias involves straightening of any chordee and then an extension of the urinary tube (urethra) out to the tip of the penis (the glans). A straight penis is necessary for satisfactory sexual function. Although this may not seem to be an important matter in childhood, this is a crucial concern later in life.
Surgical Correction of Hypospadias and Chordee
There are many operations used for the treatment of hypospadias. Fortunately, the techniques have improved dramatically decreasing the number of operations needed to correct this condition. When the operation is completed, any extra skin is removed so the child will look circumcised. It is recommended that the children have surgery to correct hypospadias at about 6 to 8 months of age. Although we try and correct most children with one operation, some of the more severe cases are best managed with two surgeries. A small number of patients may also require a second surgical procedure to manage complications of the surgery. If that is necessary, the second operation is delayed for 6 to 12 months by performing the first operation early in life then both operations can be completed before the child completes toilet training. Correction of hypospadias is performed on an outpatient basis under general anaesthesia. Depending upon the severity of the hypospadias, some children will need to go home with a catheter that drains urine from the bladder and allows the new urethra to heal. This tube will be left in place for one to two weeks. This will drain into the baby’s diaper until it is removed. We also leave a bandage on the penis. Due to the nature of the surgery, there can be considerable swelling and discolouration of the penis for a period of time after the surgical repair.
Complications
Infection of the skin and urine are few of the possible occurrences. Bladder spasms are usually due to the indwelling catheter. Medications help but do not eliminate spasms. Fistula is another risk. This is a leak of urine from somewhere along the new urethra. This risk is minimal in simple repairs but may occur 10% of the more extensive operations. Fistulas are usually easily repaired with an outpatient surgical procedure, although this is done no sooner than 6 to 12 months from the time of the original operation.
Stricture or stenosis consists of narrowing due to scar tissue where the new urethra joins the native urethra or at the new opening on the end of the penis.
Labial adhesions occur when the inner folds of the female genitalia (labia) temporarily grow or adhere together. They are most common in young girls (3 months to 6 years of age). Labial adhesions are related to hormonal influence. Labial adhesions usually occur due to inflammation of the skin which makes the labia adherent or stick to each other. Poor genital hygiene and bacteria normally present in the area may contribute to labial adhesions. Keeping the area clean and dry is important in the treatment and prevention of labial adhesions.
The majority of labial adhesions are asymptomatic. Post-void dribbling may occur due to labial adhesion. Urinary tract infections are rare with labial adhesion.
The initial treatment of labial adhesions is a trial of Estrogen cream. If this is the method chosen for your daughter, then you will need to apply the Estrogen cream 2 times per day for 2 -8 weeks as directed by your urologist. Use a pea-sized amount of cream and apply the cream to the middle of the adhesion and apply slight pressure with your finger.
Occasionally, a doctor will recommend separating the labial adhesions in the office with topical anaesthetic (numbing cream). In some children, this procedure is done under general anaesthesia in the hospital.
Once the adhesions are gone, you will want to prevent them from recurring. It is important to apply a thin layer of Estrogen cream on the area every night for at least a month.
What is Neurogenic Bladder (NB)?
NB is a term used, for a dysfunctional lower urinary tract, due to causes other than primary urinary tract pathology.
What happens in normal conditions?
Except in infants and small children, who have automatic & involuntary passing of urine, the act of passing urine is completely voluntary. Urination is initiated when a person wants to pass urine and can be controlled if the situation is not conducive. This passing of urine should be free, without the need to strain, and each time should empty the bladder. When the bladder keeps filling, the sphincters tighten and prevent a leak of urine. When the bladder contracts to empty, the sphincters open to let urine out. These work in an extremely coordinated manner. Any condition other than this, any involuntary leak of urine, or difficulty to urinate is abnormal and needs evaluation. Difficulty to pass urine, or leaking of urine can be a major social handicap or nuisance to others.
The passing of urine or controlling urination is under the control of the central nervous system. Messages from the brain are sent through the spinal cord and the lumbar and sacral nerves to the bladder and sphincters. If for any reason the spinal cord or its nerves are damaged, or the normal functioning of the brain itself is affected, this control is lost. The bladder may then lose sensation, and fail to empty, or may overwork; the sphincter may or may not open appropriately.
What conditions cause NB?
Diseases such as Parkinson’s, Alzheimer’s, multiple sclerosis, large cerebral haemorrhage, dementia, spinal cord injury /tumours/transverse myelitis, or injury to the nerves by surgery, diabetes mellitus, etc., may all cause a neurogenic bladder.
How do they present?
Such patients present with one or more of the following signs and symptoms: Retention of urine, inability to control urination (frequency, urgency), urine incontinence, loss of bladder sensation, etc. Disturbance of bowel control is also very common. These are in addition to the general symptoms of neurological injury such as coma/paralysis etc.
While physical disabilities may seem very frightening, they are usually not life-threatening. But bladder dysfunction, while not very overt, is usually the cause of severe morbidity, renal failure and even mortality. It is often neglected due to lack of awareness of its ill effects.
What are the investigations required?
The clinical diagnosis of a neurogenic bladder is made on the basis of certain simple and preliminary tests such as urine analysis, an ultrasound evaluation, MCU (micturating cystourethrogram) wherein contrast filled in the bladder and x-ray films are taken; urodynamic test in which bladder pressures and activities of the sphincters are measured during filling and voiding phase and this test will allow us to further plan his/her treatment. An MRI of the spine (see the picture below) or brain is required to look any cause in the nervous system.

How is neurogenic bladder treated?
The focus in managing a neurogenic bladder is to prevent renal damage. Renal damage occurs due to intolerably increased pressures in the bladder, causing backpressure effect on the kidneys, resulting in their slow damage without symptoms in the early stages. They also develop urine infection, stones etc. All treatment will therefore, be aimed to reduce these bladder pressures.
The treatment options will be decided after urodynamic study.
The simplest of treatment would be to teach patients to pass a catheter themselves, every 4-6 hours, depending upon the urine volumes, to keep the bladder empty and also prevent incontinence. In males and in females the technique details on how to perform are mentioned.
Medicines are also used to reduce the pressures in the bladder. Generally, the tablets will need to be taken for a lifetime, till alternative therapies can be instituted.
Surgery: is done either to reduce the pressures in the bladder by adding bowel ( small or large intestine) with an increase of capacity, or by way of inserting an artificial sphincter to prevent a constant leak of urine. Surgery is resorted to only if all other measures have failed.
Management of neurogenic bladder must include bowel management also, as an integral part of the treatment. This may include a change in dietary fibre, enemas, and laxatives.
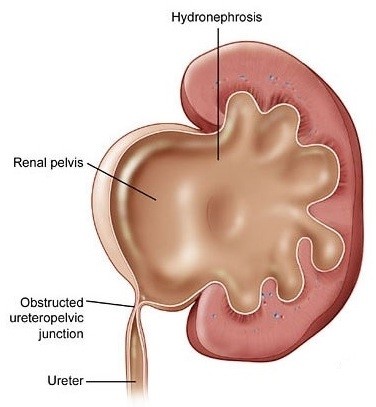
What is pelviureteric junction (PUJ) obstruction?
It is a restriction to flow of urine from the renal pelvis to the ureter, which if left uncorrected, may lead to progressive renal deterioration. The blockage is always partial but the degree of the block may vary from minimal to severe. Mild cases usually don’t impair kidney function. Severe cases can cause significant impairment in kidney function. Because it impedes the flow of urine, there is a resulting enlargement of the renal pelvis (hydronephrosis).
PUJ Obstruction (PUJO) is the most common cause (48%) of significant hydronephrosis detected on prenatal ultrasound or in new-borns.
What Causes PUJO?
Most often PUJO is congenital (present from birth), usually because of an abnormality in the development of the muscle surrounding the PUJ. PUJO can also occur later in life and can be caused by other factors, including compression of the ureter by abnormal blood vessels, inflammation, stones or a scar tissue.
What are the symptoms of PUJO?
Most infants (less than 1 year) are asymptomatic, and most children are discovered because of their symptoms. Symptoms suggesting PUJO include hematuria (blood in the urine), urinary tract infection (UTI), kidney stones, failure to thrive, pain associated with nausea and vomiting, abdominal fullness/palpable mass or hypertension.
What tests are required to confirm the diagnosis?
Due to the increased use of antenatal ultrasound (during pregnancy), if any hydronephrosis is identified, the foetus will need to be monitored throughout the pregnancy. Once the baby is born, a repeat ultrasound is to be done at least a week after delivery to confirm the PUJO.
If PUJO is affecting one kidney, then further investigations can be done when an infant is 4-6 weeks of age. These tests would include blood and urine tests to find out overall kidney function and to rule out UTI.
If both the kidneys are affected by PUJO, your Urologist may get blood and urine tests at the earliest to know the status of overall kidney function. Further course would be decided based on these reports and other details on ultrasound.
A nuclear scan (DTPA renogram or EC renogram) uses radioactive isotope which is injected intravenously (IV) and this isotope is taken up by the kidneys and excreted in the urine. Using a special camera, images of the kidneys can be seen clearly. This test gives information about individual kidney function as well as degree of blockage. This test can be done above the age of 4- 6 weeks.
CT scans are rarely required to confirm this condition and are also avoided as this involves higher radiation.
Do all cases of PUJO need surgery?
No. Following are some of the common indications:
Presence of symptoms (noted above) associated with the obstruction
Impairment of overall renal function
Progressive impairment of obstructed kidney function
Development of stones or infection, or causal hypertension
What is the aim and goal of correcting this condition surgically?
The aim is to restore non-obstructed urinary flow. The primary goal of surgery is relief of symptoms and preservation or improvement of renal function.
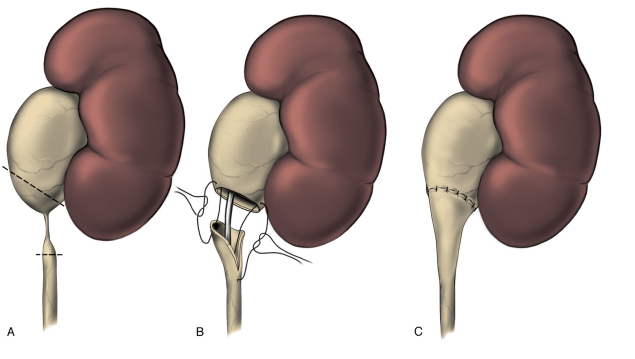
What is the surgical procedure most commonly performed for this condition?
Pyeloplasty, is a surgical procedure that removes the scar tissue from the blocked area and reconnects the healthy part of the ureter to the renal pelvis, so as to create a wide opening. The success rate is higher than 95 %. Most of the time, open surgery is performed in infants. In older children and adults the same procedure can be performed laparoscopically (keyhole surgery).
A tube called ureteric stent is usually placed to drain urine from the operated kidney across the area of repair to the bladder. In addition, you may have a bladder drainage tube (urethral catheter).
Rarely a nephrostomy tube (the inner end in the kidney and coming out of a separate small incision in the flank region) is required to drain the kidney (this is done when placement of ureteric stent was not possible). Sometimes a drain tube is placed around the area of repair (outside the kidney), to drain any blood/urine collection.
What is the dos and don’ts after this surgery?
You can have regular diet, once you are able to tolerate orally. Sometimes, especially infants will have swelling of the tummy (abdomen) and this subsides in a day or two, till then I.V. fluids would be continued.
The urethral catheter is usually removed on the 3rd day morning after surgery. And you will be allowed to go home later that evening with ureteric stent (not visible outside the body) if you are doing well. Drain tube or nephrostomy tube, if placed, would be removed at appropriate times based on clinical situation.
With ureteric stent inside, you may experience urgency, frequency, burning urination, mild blood-tinged urine and flank pain for a minute or so when you are passing urine. These are expected things, but if you have severe pain or high grade fever, do contact your doctor.
You will need to repeat urine culture 2 weeks after surgery. Based on the report, ureteric stent removal would be planned, if required under cover of appropriate antibiotics based on sensitivity.
What are the possible complications if this condition is left untreated?
If left untreated, PUJ obstruction can lead to progressive loss of kidney function, kidney stones or infection.
What is the follow up after stent removal?
Renal ultrasound is obtained 3 months after pyeloplasty to ensure that the hydronephrosis is reduced or at least remaining stable. A nuclear scan (DTPA/EC) may be obtained 1 year after the pyeloplasty to provide a relative assessment of the overall renal function and drainage pattern.
When do you say surgery is successful?
Improvement in hydronephrosis on ultrasound and stabilization or improvement in function on nuclear scan (DTPA/EC). If the patient had a symptomatic presentation, resolution of flank/abdominal pain or vomiting should also occur.
What are the other complications of surgery?
Less than 5% of patients may have a recurrence of narrowing at the PUJ requiring redo surgery. Urinary leakage from the area of surgery may require placement of a percutaneous drain. Other problems include wound infection and hernia which are very rare.
Regular examination of the testicles should be a routine part ‘of the health program of every adult male. The main reason for this suggestion is that cancer of the testicles is one of the more common tumours that occur in men, particularly between the ages of 20 and 40. All males should learn self-examination and make a point of checking themselves each month. Only by learning what the normal anatomy of the testicles feels like will they be able to detect any changes that might occur.
The exam should be done in a comfortable position. Some men prefer to check themselves in the shower or bathtub. The shape and position of the testicle should be inspected. On the outside or lateral surface, a groove called the lateral sulcus can be felt between the testicle and the epididymis, which connects to it. The testis normally feels firm, but not too hard.
Testicle will be badly damaged that it will have to be removed surgically. Also note that these cases early operation within 4 to 6 hours from the onset of pain, will allow the testis to be saved by untwisting the testicle and restoring the blood flow. To prevent this from recurring, usually the testis is fixed to scrotal wall and this needs to be done on the opposite side as the same abnormality usually exists on the other side. In some cases, the twisting is intermittent. All cases of acute testicular pain should be consulted to an urologist.
Torsion of the testicle is the most common paediatric urologic emergency. This usually happens because the sheath of blood vessels that supply the testicle becomes twisted or torsed. In the foetus the testicle develops with the abdomen and migrates into the scrotum, trailing behind it like a leash is its blood supply. In the scrotum, the testicle resides within a smooth sac called the tunica vaginalis. The testicle can spin and move about within the sac. The twisting or torsion blocks the blood vessels, which supply the testicle with oxygen and other nutrients. When torsion has occurred and is unrelieved the testicle will be badly damaged that it will have to be removed surgically.
Sudden scrotal pain is the most common symptom. This pain is due to ischemia or lack of blood flow. This is similar to the chest pain that occurs when a patient has a heart attack. The pain is usually on one side, but it can spread and be felt in the groin, abdomen, and flank. About one in four will have nausea and vomiting. The pain can come during an activity such as sports or after minor accidents. It can come on at rest or even during sleep. Children, particularly teenage boys, are often reluctant to report testicular or scrotal pain. Hours and sometimes days can pass before they are seen by a doctor. The diagnosis of torsion can be difficult to make. Other illnesses can appear like torsion. But because torsion if left untreated, will lead to the loss of the testicle, any acute scrotal pain is treated as torsion until proven otherwise.
When testicles have been torsed they can sustain an injury. The key factor is the length of time that the blood supply is occluded. Torsion relieved within six hours or less usually results in no lasting effects. After six hours the risk of damage increases. These injuries can cause decreased sperm production and infertility issues.
The only treatment of testicular torsion is immediate detorsion and operative fixation of the testicle to the scrotal wall. Occasionally it is possible to manually untwist the testicle, but the safest and surest course of action is surgical exploration. The child is put under general anaesthesia and a small incision is made through the scrotum. The testicle is examined under direct vision. After the testis is untwisted, it is observed. If the testicle has already damaged and become black (gangrenous) it is removed. If it looks normal and healthy, it is securely sewn to the scrotal wall to prevent any further twisting. When torsion is found on one side the other testicle is also explored and secured to the scrotal wall with sutures. Experience has shown that if one testicle can twist the other one can as well. The surgery usually takes about one hour to perform, and most children are able to go home either on the same day or the next day.
Intermittent Torsion
Some boys and men will present with intermittent pain of the testicle. This can last for several minutes or a few seconds. This pain may be related to intermittent torsion of the testis. Due to the start time and span of symptoms, the findings have often resolved by the time the patient presents to the doctor. If the history is typical of torsion, the patient may be scheduled for elective fixation of the testis. This is necessary to prevent an episode of torsion which will not spontaneously resolve, thus leading to testicular damage.
Urinary frequency is a common problem seen in the paediatric urology clinic. Frequency of urination can have many causes. The initial testing performed is a urinalysis to exclude urine infection and diabetes.
The mean age of onset is about age 5 years. It comes on suddenly in many cases. This disorder is believed to be an increased awareness of bladder sensation. The child feels an intense urge to void, although they have very small volumes of urine in the bladder. There is really not much they can do to inhibit voiding and actually, this should not be done. Otherwise, the child will begin to have other problems such as wetting. Most children who have urinary frequency have good urinary control. Occasionally the frequency of urination can occur as often as every five to ten minutes. In most cases, it is a little less dramatic. Children can have increased urination during the night. However, it is found only once they fall asleep, they will sleep peacefully through the night. When they first go to bed, they may keep getting back up to the bathroom until they have dozed off.
Our evaluation of the children is limited to a good history, physical examination and urinalysis. Rarely Ultrasound abdomen with full bladder and after passing urine is done to rule out any abnormalities.
There are limited in treatment of this disorder. The medicines that are commonly used for daytime incontinence or bedwetting may not work. These medicines work on the motor component of the bladder and have no impact on extraordinary urinary frequency due to increased bladder sensation. The latter medication may be helpful because some think this could be an allergic type phenomenon causing bladder inflammation.
The most important thing is just reassurance to the child that this will improve over time. Once they began to focus on other matters, they are less drawn to the sensation of the bladder fullness. A small number of older children have had a decrease in frequency after taking the prescribed medicine for some days.
Urinary Tract Infection (UTI) in children is quite common and surprisingly not diagnosed most often. UTI occurs both in normal children and in those with some urinary tract abnormality. The reason so much of importance is laid on the diagnosis and management of this problem is because, unlike other diseases, infants who have a urinary infection may not have any symptoms pertaining to the urinary tract at all.
How common is the problem?
As many as 6% of girls and 2% of boys will develop a UTI.
What are the symptoms of UTI in children?
The common belief with most parents is that with urinary infection, the child should present with burning in the urine, blood in the urine, difficulty in passing urine, and so on. This is a common presentation in adults. But in children, these are rarely true. Less than one year of age, they may present simply with fever, not feeding well, loose stools, vomiting etc., Unless one has a high index of suspicion about the presence of a UTI, it can be missed.
What causes UTI in children?
Infection commonly occurs as a result of bacteria ascending from the genital area. Girls have a higher incidence in their early years because of the short urethra. There may be numerous other causes contributing to be the incidence of infection, in which either the flow of urine down from the kidney may be blocked at different levels, or the normal flow of urine out of the bladder is disturbed, with urine going backwards into the kidney.
How is UTI diagnosed in children?
Those children, who have a fever of unknown cause, must have a urine test done. It costs very little even in a private clinic, and will give a very good indication if urinary infection is present. Once urine infection has been detected, all children must undergo further tests like a urine culture, and further testing will be decided by your doctor. These include ultrasound abdomen evaluation, an MCU (Micturating cystourethrogram) X-ray to find out abnormality in the urinary tract, and decide on treatment. Additional tests include nuclear scans which are a special type of imaging of the kidneys to look for any evidence of scarring. In this, a small amount of radioisotope tracer is injected in the arm vein. The isotope will be taken up by the kidneys and scan will give information about kidney function and also the presence of any scars.
How is UTI treated in children?
UTI is treated with antibiotics. After giving urine culture, your doctor will choose an antibiotic drug which has to be taken either orally or intravenous route. Based on the culture report, which comes usually after 48 hours, the antibiotic may be changed. The course of antibiotic will be decided by your doctor and maybe given up to 2 weeks.
Can UTI be prevented?
Certain habits are useful to prevent recurrent urinary tract infection if a normal urinary tract is found on evaluation. Adjusting fluid intake to age and bladder capacity and frequent bladder emptying will help clear infection from the bladder. Avoiding constipation by a high fiber diet or medications is very important.
Does UTI have long term effects?
Young children are at significant risk for kidney damage due to urinary infection, kidney scarring occurs, which is the most serious long term result. This in turn, leads to protein leak in the urine, high blood pressure and decreased kidney function. Those who have had infection very early in their life will have severe scars in the kidney.
The goal is the early detection of urinary tract abnormalities and the prevention of kidney infection by either medical or surgical means. Long-term studies have shown a 10% incidence of kidney failure, 13% incidence of high blood pressure, and another 13% incidence of kidney-related problems during pregnancy. When one considers that renal scarring is the fourth leading cause of renal transplantation in children, the need for prevention becomes obvious.
Urinary Tract Infection in Children
Symptoms of voiding dysfunction such as the following occur frequently in childhood and are a common cause for parental concern.
- Frequent voiding (frequency)
- Urgent need to void (urgency)
- Wetting (incontinence, enuresis)
These symptoms are normal in the very young and are usually due to an immature bladder. Young children need diapers because reflex voiding and involuntary bladder contractions result in wetting. Toilet training and a successful transition to an adult type of bladder control depend on the maturation of 3 functions.
First, the bladder capacity must increase and second, the child must develop voluntary control over the sphincter muscle in order to start and stop voiding. Next, the child must develop voluntary control over the infantile voiding reflex which allows the child to stop involuntary bladder contractions. Usually, by the age of 4 years, most children have developed the adult pattern of bladder control. At this point, the child will have no involuntary bladder contractions while the bladder fills with urine. Also, the sphincter muscle will tighten as the bladder fills and voluntary bladder contractions will cause the sphincter muscle to relax resulting in complete bladder emptying.
During the period of time when the child is making the transition from an infantile to an adult pattern of bladder control, almost every child will transiently display some symptoms of a voiding disorder. One must be cautious about over-interpreting symptoms which are transient and a normal part of the bladder maturation process. However, when symptoms of voiding dysfunction persist after toilet training, then anatomic or neurological causes must be excluded. The goal in evaluating symptomatic children is to differentiate between those children whose voiding symptoms are only due to a delay in normal bladder maturation versus those children with significant urological or neurological abnormalities. The initial examination includes a history and physical examination as well as a urine examination. Families will frequently be asked to keep a diary of a child’s voiding habits so that an accurate determination can be made of how often a child voids and at which time in the voiding cycle the child has an episode of incontinence (wetting). Many children’s symptoms will resolve when their attention is focused on their voiding habits solely by keeping a detailed enuresis diary.
Certain physical findings and symptoms may require further diagnostic studies beyond the initial office evaluation. These include lumbosacral spinal abnormalities on physical exam, as well as a history of urinary tract infection, difficult or painful urination, and persistent day and nighttime wetting. Further investigative studies will be individualized depending on the particular child’s history and physical examination. The initial imaging test is usually an ultrasound study of the kidneys, ureters, and bladder. This study looks for abnormal dilation of the upper urinary tract or hydronephrosis. A voiding cystogram (x-ray) will be recommended for some children in order to evaluate the lower urinary tract. This study shows the anatomy of the bladder and urethra and evaluates bladder emptying. The initial evaluation and additional imaging studies will identify those children with complicated conditions who may require surgery or additional specialized evaluations such as a neurosurgical evaluation.
The majority of children who display symptoms of urgency, frequency, and/or enuresis have an immature bladder for their age and treatment can be started after the initial evaluation. Many children do not heed the bladder’s message that it is full and develop enuresis due to a delay in using the bathroom. This leads to the frequent complaint of parents that their child does not have any sensation of the need to void. Most of these children will display signs of a full bladder by squatting, grabbing themselves, fidgeting, dashing to the bathroom at the last minute, etc. Timed voiding is when the child is required to void at a predetermined interval which is based upon the child’s history. Initially, it is usually recommended that the child void every 60 to 90 minutes. The interval is increased as success is achieved. A timed voiding schedule has great success in treating wetting due to a delay in voiding. In some cases, a pocket timer is indicated to remind the child to void. Children with urgency and frequency who cannot make it to the toilet on time, which leads to wetting accidents (urge incontinence), will respond in may cases to anticholinergic medication. These medications, such as Tolterodine, cause relaxation of the bladder and decrease the feeling of urgency which helps prevent episodes of urge incontinence. Anticholinergic medications can cause facial flushing and dry mouth. These are not allergic reactions but are side effects of the medication.
The use of a timed voiding schedule and anticholinergic medication is aimed at treating daytime symptoms. In many cases, anticholinergic medication needs to be used only for a short period of time, such as 3 or 4 weeks. A child’s voiding habits may respond relatively quickly to the recommended treatment plan. However, some children do regress periodically, especially at times of stress such as at the beginning of a new school year, etc. In those children with day and nighttime enuresis, these treatment modalities may have little effect on nighttime wetting. The goal is to remedy the daytime symptoms first and then treatment of the nighttime wetting would be indicated. Treatment for nighttime wetting includes the use of a bed alarm system or vasopressin (DDAVP).
Children with significant behavioral problems may show little response to urological treatment programs and may benefit from behavioral counseling. Children with developmental delays will frequently demonstrate a delay in toilet training due to a persistent immature bladder.
In children with significant daytime voiding symptoms who are refractory to treatment, special testing of bladder function may be indicated (urodynamic studies). This examination measures bladder and sphincter pressures during bladder filling and emptying. The results of the urodynamic testing may indicate different forms of treatment are indicated.
Ultimately, most children with uncomplicated enuresis will develop adult urinary bladder control as the bladder matures with time.
Meatal Stenosis is an abnormal narrowing of the urethral opening (meatus). If the narrowing becomes significant, urine will have difficulty flowing from the bladder and may cause the bladder to not empty completely.
Meatal Stenosis occurs in circumcised boys. One theory is that the stenosis is caused by the chronic exposure of the irritating effects of urine on the meatus and rubbing of the meatus on a diaper or clothing. This causes inflammation that can lead to scarring.
Symptoms of meatal stenosis include, but are not limited to:
1) Painful urination
2) Straining to urinate
3) Frequent urination
4) Decreased caliber (thin) urinary stream
5) Spraying with urination
6) Upward deflection of the urine stream
7) Blood in the urine
Treatment of meatal stenosis
is
done
by one of 2 methods. In meatoplasty, the
meatus
is
opened or widened by making an incision in the urethral
opening
and placing a vascularized flap usually from prepuce or
surrounding penile skin to prevent recurrence of
narrowing.
In meatotomy, the meatus is opened or
widened by
making a small incision in the meatus and cut margins
are
either
sutured with dissolvable sutures or left alone to heal.
The
ideal treatment plan for your son will be discussed with
you
by
your surgeon. Some children may require dilation of the
urethral
opening after these procedures. This is done to prevent
recurrence of the narrowing.
Main Reasons for These Operations
In some conditions such as Spina Bifida or posterior urethral valves or bladder exstrophy, the bladder becomes very small and holds the urine at high pressures.
Incontinence and kidney damage are typical results of such abnormal bladders. For these patients, relief of their symptoms and protection of the kidneys requires that the bladder be increased in size (bladder augmentation). In some patients, removal of the bladder becomes necessary. This would most commonly be needed to treat cancer of the bladder or other pelvic organs. For these patients, a new reservoir must be created (bladder substitution) with a pathway for drainage of the urine either through the normal channel (urethra) or through a new channel (stoma). Enlarging or replacing the bladder requires major surgery. These operations require the use of intestine to replace the bladder. The intestine is opened and reconfigured to create a normal-appearing bladder. After surgery, the bowel needs to rest for several days before the patient can be fed. This usually requires a tube placed down the nose into the stomach to drain intestinal fluids and air.
Problems Of Bladder Augmentation And Substitution
Catheterization: The intestine doesn’t function like the normal bladder. All patients need to use intermittent catheterization to empty their bladder.
Mucus Formation: The intestine produces mucus. The normal bladder does not. This mucus can cause obstruction of the catheters that are draining the bladder immediately after surgery. The catheters are irrigated several times daily to prevent this occurrence. Long term, the mucus needs to be evacuated daily from the bladder, or else the mucus that stays in the bladder is a source for development of bladder stones. It can also promote infection of the bladder. Over a period of time, the mucus production will decrease, but it will still remain in minor quantity.
Intestinal Complications: Early after surgery, the patient is at risk for leakage of intestinal contents. This is a very rare event that can lead to serious infection. The other major risk of intestinal surgery is bowel obstruction. This can be the cause of severe abdominal pain and cramping. Any of these symptoms should receive prompt.
Bladder Rupture/Perforation:
One of the most serious complications after surgery for
bladder
augmentation is rupture of the bladder. This is not
common,
but
can lead to severe abdominal infection and even death.
Most
cases of bladder rupture are due to failure to perform
catheterization on a regular basis. This leads to
chronic
over-distention of the bladder and weakens the bladder
wall
due
to ischemia. The symptoms are that of abdominal pain,
fever
and
generalized infection. The patients and their family
members
need to be acutely aware of the risk for perforation so
that
they can alert other physicians that may be treating
them to
the
possibility of this complication. Many clinicians are
not as
likely as urologists to suspect this
diagnosis in
a
patient who has undergone augmentation.
Bladder Cancer: Patients
that are on intermittent catheterization for neurogenic
bladder
do have an increased risk for bladder cancer. Patients
who
have
undergone bladder augmentation also have a risk for
bladder
cancer.
According to the Rome IV criteria for constipation, a patient must have experienced at least two of the following symptoms over the preceding 3 months:
- Fewer than three spontaneous bowel movements per week
- Straining for more than 25% of defecation attempts
- Lumpy or hard stools for at least 25% of defecation attempts
- Sensation of anorectal obstruction or blockage for at least 25% of defecation attempts
- Sensation of incomplete defecation for at least 25% of defecation attempts
- Manual maneuvering required to defecate for at least 25% of defecation attempts
Constipation is very common in children with urinary tract infections, daytime wetting and night-time wetting. Treatment of constipation includes education, prevention of impaction, promotion of regular bowel habits and toilet training in older children. Constipation is not a life-threatening condition. However, several months to years of supportive intervention may be required for effective treatment.
Daily bowel movements are a mainstay in treating constipation. The goal for your child is a soft bowel movement every day. You may help your child attain this goal by providing a daily stool time (ideally, 15 to 20 minutes after eating to take advantage of the gastrocolic reflex). Do not rush- allow your child plenty of time in the bathroom – usually 5-10 minutes. Help your child keep a stool diary – When they have a bowel movement, make note of the consistency, soft or hard,
There are several treatments for constipation. There are several dietary measures that can improve constipation. Most important is increasing fluid intake. It is important to drink enough water to maintain clear or light yellow urine. Some foods can help constipation while there are others that should be avoided.
Some examples of foods to add or increase in your child’s diet include,
fruit juices, i.e. prune, pear, plum, pineapple, peach, papaya, apricot, orange, or apple.
Vegetables, either raw or cooked (eat the peels as often as you can).
Fruits (eat the peels as often as you can).
Bran cereal, bran muffins, raisin bran.
Bananas.
Examples of foods that may worsen constipation include;
Dairy products, i.e. milk, cheese, ice cream.
Rice or rice cereal.
Pastas, white bread, potatoes.
In many children, supplements to the diet may be prescribed to produce daily bowel movements. These include magnesium citrate, Miralax, mineral oil or Milk of Magnesia. Miralax or polyethene glycol works by holding onto water and making the stool softer. When mixed in water, juice, or soda MiraLax has no discernible taste. Dosages will be determined by your physician.
Management of constipation requires considerable patience and effort on both the child’s and the parent’s part. Providing support and encouragement during the treatment period is extremely important. Multiple clinic visits may be required until appropriate laxative dosage has been established, as dosage adjustments may be required. It is important to keep in mind that dietary factors alone will probably not alleviate chronic constipation if stool withholding and retention are a problem.
In some children with neurological conditions affecting the bowel and bladder, in addition to above measures may require regular enemas to clear the bowel.
A kidney stone is a solid piece that forms in the kidney from the precipitation (crystallization of previously dissolved particles) of certain substances in the urine. Stones usually form in the kidney and will either remain there or break loose and subsequently travel down the urinary tract.
Kidney stones vary in size and shape. They can range from the size of sand particles to golf ball size. Some stones, known as staghorn stones, can fill the entire kidney. Kidney stones may be smooth or jagged.
Not all kidney stones cause symptoms. A small stone may pass all the way out of the body without causing too much pain. In some cases, the stone may get stuck in the ureter, bladder or the urethra, causing pain and possibly obstruction, blocking the flow of urine out of the kidney.
Kidney stones may be caused by a number of factors, including dehydration, infection, diet, metabolic diseases, family history, medications, limited activity level, and conditions that result in an increased concentration of calcium or other substances, including oxalate and uric acid, in the urine. The most common type of stone contains calcium.
Symptoms
- Extreme pain in the back or flank area (pain is usually excruciating and comes in spasms and may radiate to the inguinal area)
- Blood in the urine
- Fever and chills (if an infection is present)
- Vomiting
- Urinary frequency or urgency
- Pain/burning when urinating
Treatment for kidney stones varies, depending on the type and size of stone and location. Stones that can’t be treated with more conservative measures may need surgery. This can include shock wave therapy (ultrasound waves break the stone called ESWL), endoscopy (use of a laser to break the stone called URS), or placing a tube into the kidney (called PCNL). Rarely an open incision is used to remove the stone (called Pyelolithotomy). Treatment for your child’s stone will be determined by your doctor at the time of your office visit.
It’s important to determine the underlying cause so that more stones aren’t formed in the future. This is done by performing tests on the blood and urine to look for factors predisposing to stone formation.
In most cases, prevention of kidney stones is simply done by increasing water intake and occasionally by making a few dietary changes. In some cases, medication may be needed.
Multicystic Dysplastic Kidney (MCDK) is the term used to describe a congenital renal anomaly that consists of a kidney completely replaced by multiple cysts that are held together by connective tissue. The kidney looks like a bunch of grapes. The ureter is often atretic or absent. The cysts often do not communicate, and this condition must be distinguished from hydronephrosis. With increasing utilization of prenatal ultrasound, the common mode of presentation has changed dramatically. At the present time, 47% are detected prenatally, 30% present with a flank mass, 5% urinary tract infection, 18% other presentations. It is more common in males and there is a slight left-sided predominance.
The diagnostic evaluation includes a renal ultrasound which shows several characteristic features that helps to distinguish a multicystic kidney from a hydronephrotic kidney. To substantiate the appearance of the renal ultrasonogram, a renal scan, DMSA, (or) MAG-3 is usually obtained. This test usually confirms the absence of renal function. In additions, this test helps to evaluate the contralateral kidney. In 18% of the cases, a contralateral renal abnormality may be encountered. In some cases, there might also be contralateral vesicoureteral reflux. For this reason, a nuclear cystogram or voiding cystourethrogram is also recommended.
If the condition is detected prenatally, it is important to visualize the opposite kidney to see whether it is abnormal. At the same time, the amniotic fluid volume should be assessed to make sure that it is adequate. If the amniotic fluid volume is markedly decreased and if there is bilateral renal disease, further steps should be taken to assess the viability of the baby. Luckily, the disease is rarely bilateral and the patients usually do well with one kidney.
The treatment for this condition is debatable. One group favours surgical removal of the kidney and the other favours observation. The risks of leaving the kidney in place include hypertension (rare) and the development of a renal tumour. Only 6 cases of renal tumours have been reported, 3 in childhood. The childhood tumours occurred at 10 months, 4 years, and 15 years; whereas, the adult tumours occurred 26 and 68 years. Based on the incidence of this disease, the risk of developing a tumour is low. If the kidney is left in place, the patient must be observed yearly with renal ultrasound and blood pressure measurement.
In rare occasions, the diagnosis of MCDK will be inconclusive despite the radiologic workup and in this situation, surgical exploration is indicated.
The most common urological problem seen in children is bed-wetting during sleep (medically referred to as Sleep Enuresis or Nocturnal Enuresis). About 10-20% of children between the ages of 5 to 6 years are known to wet their bed. It is estimated that there are around 80-110 million enuretic children in the world. Enuresis is more common in first-born children, more prevalent in boys than in girls, and is much more common if the parents have also had a similar problem or if there is a family history of the condition.
If one parent has had a similar problem, there is a 44% chance of his or her child, or children, having this problem. If both parents have had this problem, then there is a 77% chance of their child, or children, having a similar problem.
Enuresis is considered a disorder only if the child is at least 5 years of age and the problem continues more or less continuously for approximately one year. It is primary enuresis if it has been present since birth and considered to be secondary enuresis if it starts between the ages of 5 and 8, that is, after the child has been toilet trained.
Apart from the commonly faced problem of changing the sheets, bed-wetting needs to be handled sympathetically because it affects the self-esteem of the child. A positive change occurs in children who are successfully treated. Therefore, treatment is definitely worthwhile.
Enuretics who wet only at night and have no other abnormalities in their urological history, are termed to be monosymptomatic and have monosymptomatic nocturnal enuresis (MNE).
They must be distinguished from children who have both night-time incontinence and daytime symptoms such as urgency, frequency or incontinence
Approximately 25% of children who attain initial night-time dryness by the age of 12 years, relapse and wet for a period averaging 2.5 years..
Nocturnal enuresis has a spontaneous resolution rate of 15% per year so that, by the age of 15, it persists in only 1% of the population.
MNE is a symptom rather than a disease. A number of theories have been proposed which include behavioural, genetic, developmental, neurologic, psychological, urodynamic and organic causes. There is no single explanation for this symptom and an individual factor, or multiple factors, may be operating.
Clearly, the vast majority of children with MNE do not suffer from psychiatric, neurologic or urological disturbances and therefore investigation and treatment along these lines is both inappropriate and unrewarding.
There could be several causes for MNE in children:
For Sleep Enuresis: A number of treatment modalities have been used to treat nocturnal enuresis. However, their effectiveness, even in control studies, has been difficult to assess because of the high spontaneous resolution rate and the extremely high placebo improvement effect, which can exceed 65%.
Therapy generally follows two lines – drug therapy and behavioural modification.
Parents have different attitudes and expectations about bed-wetting and its cure. Treatment for MNE should generally be discouraged before the age of 7 years because even the success rates for treatment before this age are very poor.
Urodynamic Findings: Bladder overactivity does not occur in children with MNE at a higher rate than in normal subjects, and in most enuretic, bladder overactivity are not the cause for bed-wetting. Consequently, therapy for eliminating bladder overactivity is generally ineffective. However, the single most important observation in MNE is a reduced bladder capacity. This reduction is functional and not anatomic. It is not the cause for enuresis, although it often increases coincidentally with a cure. Those children who have daytime symptoms of frequency, urgency or even incontinence, will have bladder overactivity.
Sleep Factors: Sleep patterns of enuretic are not different from those of normal children. Most enuretics neither have a disorder of arousal nor wet as a consequence of sleeping too deeply. Instead, findings support the concept that enuresis is related to a delay in CNS development, or more accurately, a dual delay in the development of perception and inhibition of filling and contraction of the bladder by the CNS (Central nervous system).
Alteration in Vasopressin Secretions: Vasopressin is pituitary hormone also called as AVP (Arginine vasopressin). About 50% less urine is normally excreted during the night than during the day. In many children with enuresis, the circadian rhythm (biological sleep –wake cycle) of plasma vasopressin secretion is altered, with no decrease in AVP during the night. This causes them to produce larger amounts of dilute urine at night. Administration of vasopressin will be helpful only in those children in whom this increased nocturnal urine output has been documented. Studies indicate that the circadian rhythm of AVP matures over time, and it indicates that enuresis associated with AVP-induced nocturnal polyuria may simply represent another manifestation of developmental delay.
Developmental Delay: All the seemingly unrelated alterations in urodynamic function, sleep, AVP secretion, etc., that have been mentioned above, all occur normally in infants and young children and actually represent a varied expression of neurophysiological immaturity. In most children, MNE represents a delay in development, and each of these physiological alterations tends to improve with time and to resolve spontaneously.
Organic Urinary Tract Disease: Most children with MNE do not have an organic urinary tract cause for their wetting. The incidence of an organic urinary tract cause is less than 0.4%. MNE should be distinguished from enuresis associated with daytime symptoms. Such children, especially boys, should undergo urinary tract imaging with an ultrasound to search for signs of possible obstruction.
A detailed history, physical examination and urine analysis are sufficient for most children with primary MNE. The goal is to identify those children who require further study. History of urinary tract infection, day time symptoms, obstructive symptoms or certain signs of neuropathy must be pursued. In their absence, there is generally no indication for radiographic study or cystoscopy.
Due to excessive use of ultrasound screening in pregnancy now-a-days the number of children with urinary tract abnormalities who are diagnosed prenatally is increasing. Approximately 20% of foetal anomalies discovered on ultrasound involve the urinary tract. Because the diagnosis of foetal hydronephrosis is being made more frequently, the need for a coherent approach to the diagnosis and management of these patients is readily apparent.
The following are the various types of treatments:
Pharmacological Therapy:
DDAVP: Desamino-D-Arginine VasoPressin (otherwise called Desmopressin) This drug, administered in the form of a nasal spray, has been effective in about 25% of cases. It works by reducing the urine output at night. The usual clinical dose is between 10 and 20 mcg per night for the nasal spray and 200 to 400 mcg per night for the tablets. The therapeutic effect of DDAVP is temporary. Once the treatment is stopped, 50 to 90% of children relapse and resume their original pattern of wetting.
Behavioural Modification: Behavioural modification should be considered as the first line of management in enuresis. Bladder training, responsibility reinforcement, conditioning therapy using the urinary alarm, are all a part of this management – the last being considered the most effective approach available for nocturnal enuresis.
The following are the recommendations for the most effective evaluation and treatment plan:
Screening for Urinary Abnormalities: The doctor should screen for any possible urinary abnormalities. If something is found, a referral can be made to the urologist.
Reduction in Liquid Intake: All children should decrease their liquid intake by one-half of normal levels starting from evening onwards.
Avoidance of Caffeine: Most children should avoid caffeine.
Adequate Sleep: Children should get adequate time in bed. The average 8-year-old needs about 10 hours of sleep per night.
Use of an Alarm at Night: An alarm should be used to wake up the child so that he or she can pass urine at night. Due to positive reinforcement should be provided to the child for dry nights. Parents should not punish children for this problem.
Changing of Bed Linen: To help them have a positive outlook, children may be made to change their bed linen when wet. Do not use diapers for children with this condition.
Progress Chart: A progress chart will be a good record for these children.
Urination Before Going to Bed: Children should urinate just before going to bed.
For Further Information:
Please go to UrologyHealth.org (https://www.urologyhealth.org/) – a patient education site written and reviewed by urology experts in partnership with the American Urological Association Foundation.
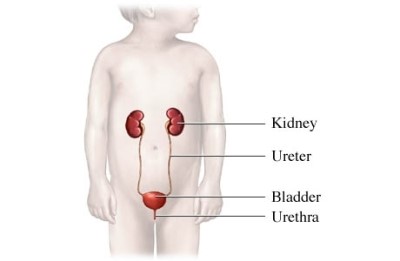
Children who are born with spina bifida frequently have abnormalities of the urinary tract. The urinary tract consists of several components
The kidneys are the organs that are responsible for filtering waste products from the blood stream and produce urine continuously. The urine drains down tubes called ureters to the bladder, which normally stores urine and empties intermittently by muscular contraction. The urine exits the bladder through the urethra. This process is called voiding or urination.
The proper filling and emptying of the bladder requires an intact sacral spinal cord. To achieve urinary control, one has to be able to feel bladder fullness. This signal is transmitted to the spinal cord and then to the brain. In an older child or adult who has normal urinary control, the brain is able to inhibit the bladder from contracting until it is socially acceptable.
In many children with spina bifida the nerves to the bladder that control this reflex voiding are damaged. Only about 5 to 10% of children with spina bifida have normally urinary control and are able to toilet train and void spontaneously. The remainder of the patients have some abnormality. This can result in poor urinary control and incontinence. More importantly, the neurogenic dysfunction can lead to damage to the kidneys and bladder. Evaluation of the urinary tract is done shortly after birth. We obtain a renal ultrasound of the kidneys in new-borns with spina bifida. There is an increased incidence of congenital abnormalities of the kidneys in children with spina bifida and these need to be recognized early in life. It is also important to obtain an ultrasound in a newborn, so that we can later determine if there has been any damage to the kidneys from the abnormal bladder function. We also will obtain an x-ray of the bladder called a voiding cystourethrogram. This is done to assess for reflux (or backing up) of urine into the kidneys. We also can evaluate the bladder Capacity and urethra.
The most important evaluation by an urologist in children with spina bifida is urodynamic studies of the bladder. These are also called cystometrogram. This study involves placing a catheter into the bladder and filling the bladder with water. While this is done, the pressure in the bladder is continuously monitored. We can also measure the pressure in the urethral sphincters (the muscles that control urination). The results of this test can predict for us very accurately whether the child is at risk for developing renal damage. The critical measurement is the pressure in the bladder at which time the urine begins to leak out around the catheter when the bladder is filled. In about half of the children with abnormal function, we find that a very high pressure develops before the urine begins to leak from the bladder. If this pressure is higher than 35 cm H20, then it will result in back pressure on the kidneys. The ureters that drain the urine from the kidney to the bladder are not strong enough to transport urine to the bladder when the bladder pressure is consistently higher than 35 cm H20. If these children are left untreated they will later develop Kidney problems.
Management Of Neurogenic Bladder
Low Leak Point Pressure (<35 cm H20)
Children that are able to leak urine freely from their bladder when it is filled during the urodynamic study (pressure less than 35 cm H20) can be followed expectantly. We will repeat the urodynamic studies at about age 6 months and then again in one year. These children usually do quite well and are at low risk for infections or any other kidney problems. They will be followed with renal ultrasounds on an annual basis for the first couple of years of life.
High Leak Point Pressure (> 35 cm H20)
Infants who are found to have high bladder pressures at the time they leak urine during the urodynamic study require early treatment. Most of these children can be managed quite effectively with intermittent catheterization. The bladder is emptied every four hours with a small tube. This is done with a clean technique. The catheter is just washed with soap and water and then rinsed carefully. The catheterization is only done every four hours during the daytime. We generally do not require that this be performed during the night-time. Many of these children will also need to be placed on medication to lower the bladder pressure.
Spontaneous Voiding
About 5 to 10% of children with spina bifida will be able to void on their own. When we recognize this in the newborn, the child still needs to be followed very closely. As the child grows, they can develop tethering of their spinal cord due to scarring. This can affect bladder function. For this reason, until the child is toilet trained, we periodically repeat the urodynamic studies to look for any loss of bladder function.
Urinary Tract Problems:
Urinary Tract Infections
Urinary tract infections are common in children with spina bifida. They occur more frequently in those patients who have high bladder pressures particularly if they are not being managed appropriately. In children who are on intermittent catheterization, we frequently see bacteria in the urine. This surprisingly causes little problem for most patients. We generally do not recommend treating the bacteria unless the patient develops symptoms. This can include pain in the bladder area, fever, blood in the urine, increased wetting or occasionally a foul odour to the urine. The most important aspect of preventing urinary tract infection in children with spina bifida who are on intermittent catheterization is to be sure that the bladder is emptied at frequent intervals. Also, we need to maintain a low bladder pressure in these patients.
Incontinence
- Surgical Management of High Bladder Pressure:
- Medical Management:
- Surgical Management of Incontinence:
Temporary measures can also be used to help lower bladder pressure. This includes cutaneous vesicostomy, which is a temporary diversion of the urine. The bladder is opened to the abdominal wall midway between the belly button and the pubic bone. This allows the bladder to continuously drain urine at low pressure. At a later age, the vesicostomy is closed and bladder management is performed as outlined below. Again, these are temporizing procedures until more definitive treatment can be done.
As mentioned above, most children that have neurogenic bladder secondary to spina bifida require treatment for urinary incontinence. For most patients, this consists of intermittent catheterization and medications. About 50% to 60% of patients will be dry with this management alone. The medications that are used generally fall into the category of anticholinergic medication. These drugs work to counteract the activities of the bladder muscle. Because they are not bladder specific, they work on other parts of the body as well as the bladder. For this reason, side effects are common but expected. These include dryness of the mouth, facial flushing, and decreased sweating. All of these will contribute to the child having poor heat tolerance. We also see a difficulty with constipation and even rarely diarrhoea. This needs to be carefully watched because of the often present bowel dysfunction. Less commonly, children will have difficulty with drowsiness and headache. The different medications used include oxybutynin, Tolteridone. If the anticholinergic medication fails to relax the bladder, there are other types of medications that can also be used such as imipramine and Tamsulosin. These work on different aspects of the bladder muscle and may sometimes be successful.
In some children, the bladder muscle is so abnormal that it will not respond to the medication. This is more often the case if the child is not managed aggressively from birth. In such cases, if the pressure remains high despite putting the child on the maximal doses of medication, we may need to surgically enlarge the bladder which can be done in several ways. The most common procedure in the past has been enlargement with a segment of the intestinal tract. This will invariably ensure a low pressure reservoir for storing urine. However, there are other problems associated with this procedure such as bladder stones, mucous in the urine and increased infections. Another cause for incontinence in children is inadequate resistance in the sphincter area. For these children, there are also a number of surgical treatments available. This can include a pubovaginal sling, periurethral Defiux injection or occasionally an artificial urinary sphincter.
Some Children Hold Their Urine Too Long
Many children with wetting or infections are infrequent voicers, but they can be hard to recognize. After toilet training, parents don’t usually know when a child urinates and the intervals between urination may become surprisingly excessive. This is particularly true if a child has had urinary accidents or infections with burning. As a result, they may deliberately hold back on urinating. The result is stagnation (resulting in bacterial overgrowth) or spillage from an overfilled bladder.
You Can Lead a Horse to Water
It is almost impossible to make children void (pass urine) if they don’t want to do so. Furthermore, if a child has a lot of emotional pressure or fear of punishment they may be unable to relax sufficiently to void effectively. Normal urination requires relaxation of the pelvic floor coordinated with contraction of the bladder muscles. The pelvic floor, like your biceps, is a muscle that you can voluntarily move, but the bladder muscle (like your heart or intestine) is an automatic muscle that you cannot order around. Normal voiding requires relaxation, not pushing and straining.
Voiding Habits (GIRLS):
Sit back on the toilet
Foot support if necessary
Relax, don’t strain or push knees apart
Take your time
When you are finished, relax and try again – there may be more urine to empty
Voiding Habits (BOYS):
Open the pant zip completely
Relax, don’t strain, push or rush
When finished, wait a moment and try again
Sit if it helps
In a Timed Voiding Program, you will try to relearn to empty the bladder when it’s time to go, rather than waiting until you have to go (because by then it may be too late!). Voiding is done by the clock or by a schedule. The idea is to keep the bladder empty, so the urine will be less likely to leak or to get infected. Usually, the timed voiding program is necessary only in the daytime. When at home or at play an alarm watch or alarm on the mobile phone may be a good way to remember when it’s time to void. During school, however, it’s better to establish a schedule such as: go to the bathroom as soon as you get to school, go to the bathroom at the midmorning break, go to the bathroom at the start of lunchtime, go to the bathroom in mid-afternoon, go to the bathroom just before leaving school, once at home go by the clock => every three hours. When following this program, the voiding habits described above are important so that the bladder can be thoroughly emptied without straining.
Sometimes people will say that they “cannot void” or “do not have to void”. This is rarely the case because everyone makes urine continuously – so if the bladder has not been emptied in the past three hours there will be at least 100 ml to 200 ml of urine in almost anyone. The job is to learn to relax when it’s time to urinate.
The testicle is responsible for the production of the male hormone and also sperm. The term undescended testicle is used when a testicle cannot be found in its normal position in the scrotum. Before the child is born the testis migrates down from high in the abdomen and passes through the abdominal wall and groin to take its normal position in the scrotum. Up to 4% of term infants will have an undescended testicle, with an even higher incidence in premature males. Spontaneous descent into the scrotum will occur in three-fourths of undescended testicles during the first three months of life.
Most undescended testicles are palpable in the groin, but some are nonpalpable, being intra-abdominal or absent. Retractile testicles are not truly undescended but withdraw into a position outside of the scrotum because of a hyperactive cremasteric reflex. Retractile testicles can be manipulated into the scrotum, but some go on to become undescended as the child grows.
INDICATIONS FOR TREATMENT OF UNDESCENDED TESTICLES
In humans, the scrotal location of the testicles keeps them 2 to 3 degrees Centigrade cooler than the core body temperature. This lower temperature is important for the development of the testis as well as for the production of fertile sperm. Studies have shown that there is an increased risk of infertility in men with a history of undescended testis. Relocating the testis into the scrotum may decrease the risk of fertility problems, particularly if done at an early age. There are other advantages to a location within the scrotum. There are a cosmetic advantage and treatment of the undescended testicle also alleviates any psychological effects resulting from an empty scrotum. The scrotal testis may be less amenable to injury than a testis outside the scrotum in that the latter may be anchored in a position directly over the pubic bone.
Finally, and perhaps as important as any other reason, a testis that has not made it into the scrotum is not accessible to physical examination. Undescended testicles are at increased risk for testicular cancer. Although testis cancer is uncommon, it is the most common solid tumour in men up to age 40 years. Testicular carcinoma is highly curable when detected early, and the best way to do this is monthly self-examination which is only feasible in testes that lie within the scrotum.
Treatment for the undescended
testicle can be undertaken any time after 6-9 months of
age.
Hormonal treatment for an undescended testicle may be
considered, but the success rate is below 10% when
retractile
testicles are excluded from the treatment groups.
Hormonal
therapy is contraindicated in children with a clinically
apparent hernia. The surgical treatment for an
undescended
testicle is called an orchiopexy.
Palpable
undescended testicles are found through a small inguinal
skin
incision. Most undescended testes are associated with a
hernia
that must be repaired. After the hernia is repaired and
we
have
obtained adequate length of the spermatic cord (blood
supply
to
the testis), the testicle is tunneled into the scrotum
where
a
small pouch is made for the testicle through a small
scrotal
incision. This operation requires general anaesthesia
but is
performed in an out-patient setting.
Nonpalpable undescended
testicles
require surgical exploration, since there is no reliable
x-ray
imaging study that can prove the absence of a testicle.
And
this
is done by diagnostic laparoscopy, where in a small cut
is
made
in the abdomen and telescope is inserted to identify the
presence or absence of testis in the abdomen. If testis
is
found
further steps are done to mobilize the testis to bring
it to
the
scrotum. Some boys will be found to have very small
abnormal
gonads which will be removed. The procedure is called
orchiectomy.
Most
of
these children probably had torsion or twisting of the
testis on
its blood supply prior to birth that led to the small
testis.
When a boy is left with a single functioning testis we
may
recommend anchoring it to minimize chances of losing it
to
torsion later in life.
What is urotherapy counselling?
Urotherapy is a non-invasive recommendation traditionally used in the management of dysfunctional voiding and irregular bowel movement habits.
What is Dysfunctional voiding?
With normal urination, the urethral sphincter relaxes and opens out when the bladder muscle squeezes, allowing urine to pass out of the body freely.
In those with dysfunctional voiding, the urethral sphincter does not relax when the bladder muscle squeezes, making it difficult for urine to be expelled out against an obstruction. This will increase the bladder pressure and change the micro organic climate of the urinary bladder thereby resulting in urinary tract infection.
What happens in an irregular bowel movement habit?
An irregular bowel movement will result in impacted stool in the rectum which compresses the bladder, reduces its functional capacity, and provokes earlier sensation to void. In addition, to retain stools in the rectum, there will be chronic pelvic floor spasm which also prevents complete relaxation during voiding, and can result in post void residuals. As the pelvic floor muscles are common to both the urine outflow and bowel control, this can aggravate dysfunctional voiding.
Why is urotherapy done?
The primary aim of the therapy is to normalize the bladder and bowel function. This therapy also aims at improvement of quality of life.
What does urotherapy involve?
Urotherapy involves the following:
Maintaining urine storage volumes to within the safe capacity of each individual’s bladder.
Emptying the bowel regularly so that the impacted stool does not exert pressure over the urinary bladder and also facilitate pelvic muscle relaxation. Maintaining void volumes/timings to safe limit, so as to let the pelvic/urethral muscles relax periodically.
Use of medications like anticholinergics and laxatives, if required.
Who performs this therapy?
Your doctor or a trained nurse counsellor will explain to you all the recommendations after assessing your clinical condition.
What are the recommendations?
In fact, recommendations will depend on the assessment results of your doctor/nurse counsellor. They may be as follows:
Tailoring of fluid consumption according to age, occupation, daily activities, and climatic condition to prevent the bladder become over distended frequently. This includes all kind of drinks also, like coffee/tea, milk, juice etc. Your doctor/nurse counsellor will tell you how much of fluid is to be taken for a day. This should be distributed over 24 hours.
Restriction of fluid consumption in the evenings to decrease the overnight urine output would be another advice.
Timed urination in the daytime. Practising timed emptying of the bladder every three hours will keep the urine stored in the bladder at low pressures. You may have to do that with an alarm, if you are likely to be engaged with work.
Pass urine before going to sleep and immediately on getting up.
Pass urine once in the night. Use an alarm to wake you up three hours after you go to bed
Maintain an interval of 2 hours between dinner and sleep, to facilitate removal of dietary liquids.
Increase the fibre content of food in the daily diet. It includes:
All unrefined/unsieved cereals (Roti, Chapati)
All Dhals, Beans, Lentils (whole- grams, sprouted grams), fresh peas
Green leafy vegetables, Raw vegetables (should be just cooked, not over cooked)
All fruits with edible portion of peel/skin
ensure you pass stools daily, at fixed times, preferably before you get occupied with the day’s activities.
What next?
You will be asked to come back after a certain period, usually one month, with 3 days of bladder diary to judge your compliance to our advice. A bladder diary records the time you get up and the time you go to bed, fluid intake, frequency of urination, urinated volumes and other information such as degree of urgency, episodes of leak etc. You will be trained by your nurse counsellor on how to maintain a bladder diary.
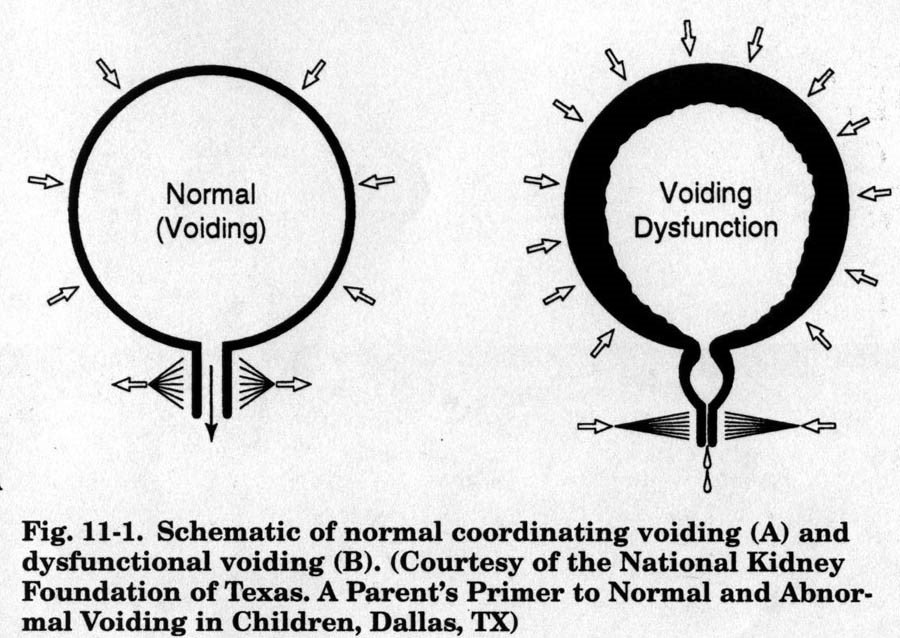
A varicocele is an abnormal dilatation or enlargement of the veins within the spermatic cord which drain blood away from the testicle. It is usually noticed as a painless enlargement of the scrotum. Some patients do notice a discomfort, heaviness or “dragging feeling” in the scrotum. On examination, the dilated veins along the cord above the testicle feel like “a bag of worms.” When the patient lies down it will make the varicocele empty and it will become smaller. Standing him up will cause it to fill and enlarge.
A varicocele is uncommon in children under 10 years of age. It becomes more common after puberty and occurs in 16% of adolescent boys. It is usually found on the left side. The exact cause of a varicocele is not known.
Varicoceles have been associated with infertility. 20-40% of men seen for infertility are found to have a varicocele and low sperm counts. On the other hand, majority of men with varicoceles have normal sperm-counts and are fertile. It is thought that the large, dilated veins cause an increased temperature in the testicle which impairs sperm production.
Based on our present knowledge and abilities, it is not possible to predict accurately which boys with a varicocele will have problems with fertility later in life. However, if the testicle on the side of the varicocele is smaller or is not growing normally compared to the other side, we do believe that this is a sign of ongoing damage to the testicle and the varicocele should be repaired. If the varicocele is very large and causing pain, then it should be corrected. If there are no symptoms and both testicles are normal in size and growth, no treatment is necessary.
Of the various methods of treating varicocele, the least invasive, higher success rates and lesser complications are with microsurgical subinguinal approach making a small incision at root of scrotum. Using an operating microscope, the surgeon can identify these veins better and ligate. This may have to be done on one or both sides.
Understanding VUR:
Your child has a condition known as Vesicoureteral Reflux (VUR). There are treatments that can help. In this brochure, you will learn about VUR and how it can be treated.
What is VUR?
Urine is produced in the kidneys. Normally, it only flows one way: down the ureters and into the bladder. VUR occurs when urine flows back to the kidney from the bladder through the ureters. This can happen on one or both sides.
What causes VUR?
About 1% of children in the world have VUR. The backward flow can be either due to an intrinsic defect in the valve mechanism at the junction of the ureter and bladder (primary reflux, or it can be because of other causes in the bladder and the outflow urinary tract (secondary reflux). In secondary reflux, the reflux resolves when the causative problem in the bladder or outflow tract is treated.
Primary reflux will need to be dealt with on its own merit. In older children, infrequent or incomplete urination, and associated constipation, are significant contributors to VUR.
Is VUR serious?
Reflux by itself is not a serious problem, does not cause infection, and does not cause renal damage. Reflux is considered important to manage, because of its association with urinary infection, and thereby renal scarring, hypertension, or even renal failure. The greater the degree of reflux, the greater are the chances of the kidneys being affected. The grade of reflux can be assessed by doing an MCU, and is graded from I (mild) to grade V (severe). Most of the time, grade I and II VUR (mild) will resolve by itself, as the child grows. Grade III to V are less likely to resolve on their own. The chances of reflux resolving by itself, are inversely proportional to the grade of reflux, the age at detection, and associated bladder and bowel dysfunction.
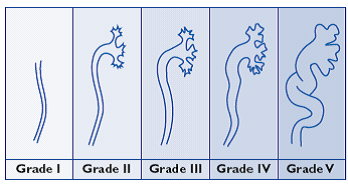
Testing for VUR
All evaluation for reflux is to evaluate for the presence or absence of urine infection, status of the kidneys, degree of reflux if present, and associated lower urinary tract function. The standard tests include, ultrasound studies which is done in all patients; a special x-ray test called VCUG (voiding cystourethrogram), which is done when the child is passing urine, and an isotope study – DMSA (Dimercapto Succinic Acid) of the kidneys to look for any scarring in the kidney.
If the parent has had VUR as a child, there is a 60 % chance that the child will also have VUR. If one child in the family has VUR, there is a 30 % chance, that the siblings may have it too. For these reasons, it is important to discuss the testing options with the doctor.
Who should be tested?
Any child with urinary tract infection should be evaluated. Which of the tests will be done for each child, again will depend upon the age of the child, the presenting symptoms, and the report of the ultrasound study. This will vary from patient to patient.
Ultrasound studies are not reliable to detect the presence or absence of reflux.
Why should VUR be treated?
Treatment of VUR is both treatment of urine infection, as well as correction of the reflux itself. The goal of treatment of VUR is to protect the kidney from being damaged.
How do I know if my child has VUR?
Symptoms of urinary tract infections include:
* Foul smelling or turbid urine
* Fever
* Abdominal pain
* Burning or pain when urinating
* Frequent and urgent urination
* Urine infection
VUR by itself does not give rise to any symptoms. It is the associated problems that draw attention to the probable presence of VUR. These are urinary incontinence, urine infection, etc.
Infants with infection may not show these signs. Instead, they may have diarrhea, poor feeding, fever, and increased irritability. If there is any question, consult your doctor and have your child’s urine checked. Children can quickly become very sick.
There is help for VUR
It is important to treat VUR to prevent possible infections and kidney damage. There are 3 options for managing or treating VUR:
- Antibiotics may be used to prevent infections until low grade VUR resolves itself as child grows. Children must take medicine every day, and be retested for VUR on a regular basis.
- Surgery can fix the ureters to stop high grade VUR. This type of treatment cures most children.
- In Endoscopic treatment, a substance is injected where the ureter joins the bladder (in low grade VUR).
How do I decide what is the treatment for VUR?
You should discuss this in great detail with your doctor. Antibiotics, surgery, and endoscopic treatment of VUR are all good choices. Your family’s personal views are most important.
Surgery may be favored if VUR is severe or if there are other related medical conditions.
Some families find it hard to do the routine X-ray test and daily medication required with antibiotic treatment.
Your concerns or beliefs matter, therefore it is important to discuss them with your doctor. Make sure you understand the risks, benefits and follow-up of each treatment.
Is follow up needed?
Regular follow up visits according to protocol is mandatory. This should be discussed with your doctor.
Normal flow of urine
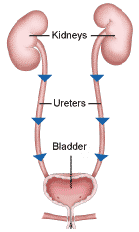
VESICOURETERAL REFLUX IN CHILDREN (VUR)